Ultrasound Identification of Common Peroneal Nerve in Order to Quickly Identify the Nerve for Targeted Muscle Reinnervation in the Lower Extremity: A Technique for Reducing Surgical Time
Rex W Hung, MD1, Kevin G. Kim, BS2, Paige K. Dekker, BA2 and Ali A Turabi, MD3, (1)Plastic Surgery, MedStar Georgetown University Hospital, Washington, DC, (2)MedStar Georgetown University Hospital, Washington, DC, (3)MedStar Good Samaritan Hospital, Baltimore, MD
Introduction:
Targeted Muscle Reinnervation (TMR) is utilized during amputation to prevent stump neuromas and/or phantom limb pain (PLP), which can be devastating consequences of below knee amputation (BKA). With incidences reported up to 67%, post-amputation pain can prevent the amputee from successful transition to prosthetics. In combination with preoperative peripheral nerve block and postoperative enhanced recovery algorithms, TMR can reduce the incidence of residual limb and PLP. Amputation and nerve coaptation are often performed by separate surgical teams, with TMR contributing significantly to surgical time compared to traditional BKA. One factor increasing time for TMR is exposure of the common peroneal nerve (CPN). In this technique, ultrasound is utilized immediately after peripheral nerve block, prior to surgery, to identify and mark the CPN to facilitate surgical dissection.
Materials & Methods:
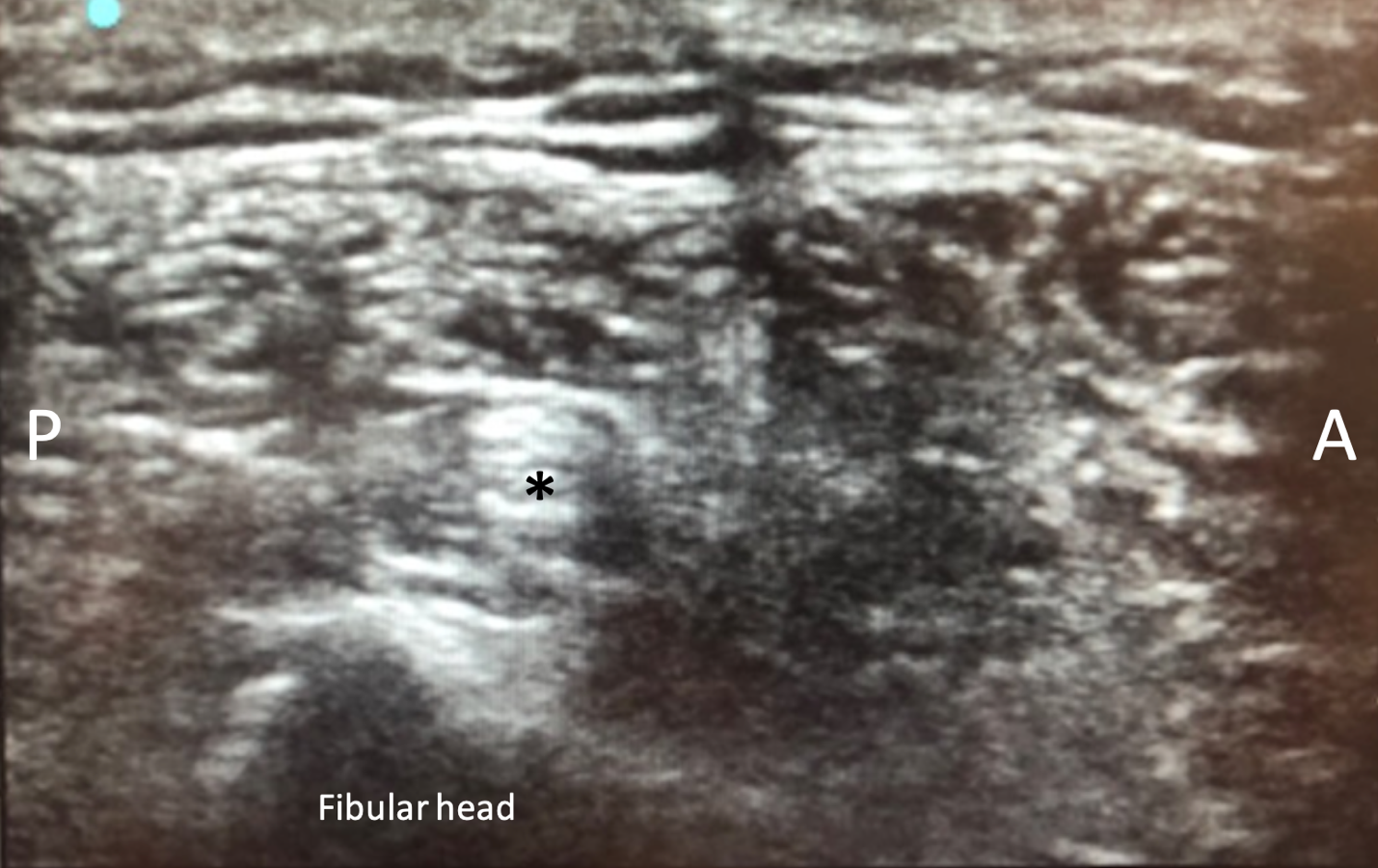
An ultrasound with a 10-5 Hz probe is used to visualize the CPN (Figure 1) approximately 1 fingerbreadth distal to the fibular head after peripheral block and prior to surgical prep. The anesthetist and peripheral nerve surgeon are both present during sonographic identification of the nerve. The skin above this area is marked with a skin marker. The depth is identified and recorded. A fiducial marker is placed in the vicinity of the CPN. The incision is designed according to the radiographically determined location of the nerve. The superficial peroneal nerve (SPN) is identified and preserved during the amputation of the tibia and fibula and creation of the posterior amputation flap. The CPN is exposed at the fibular head and decompressed. Intraneural neurolysis is performed and a nerve stimulator is used to identify a redundant motor fascicle to the extensor digitorum longus (EDL). The SPN is transposed proximally and anastomosed to the proximal end of the EDL motor fascicle. Tibial TMR is then performed to a motor fascicle to the soleus. The amputation is then completed.
Results:
The patient underwent primary BKA and the aforementioned protocol. Identification of the CPN nerve was completed and marked in 30 seconds. Mean operative time for the TMR was estimated to be reduced by approximately 5 minutes related to quicker identification of the CPN.
Conclusion:
We present a novel technique for reduction of surgical time for TMR at time of primary BKA. We found this protocol to be safe, effective, and expedient without additional morbidity.
Figure 1: Common Peroneal nerve(asterisk), under ultrasound visualization, lying along the fibular head. Anterior(A) and Posterior(P) marked.
Back to 2021 ePosters