"Even a little relief must be amazing": Peer-to-Peer Education on Social Media After Traumatic Brachial Plexus Injury
Emma Smolev, BA1, Eric Zhu, BA1, Sarah Buday, PhD1, David M Brogan, MD, MSc2 and Christopher J. Dy, MD, MPH, FACS3, (1)Washington University, St. Louis, MO, (2)Washington University School of Medicine, St. Louis, MO, (3)Washington University in St. Louis, St. Louis, MO
“Even a little relief must be amazing”: Peer-to-Peer Education on Social Media After Traumatic Brachial Plexus Injury
Introduction: Facebook groups dedicated to brachial plexus injury (BPI) are frequently used by patients seeking support and medical advice from peers. We hypothesized that a qualitative thematic analysis of BPI Facebook group posts would uncover potential sources and recurring themes of misinformation patients might encounter, thus demonstrating opportunities for patient education efforts.
Materials and Methods: The two most popular open membership BPI Facebook groups were identified by searching “traumatic brachial plexus injury”. Posts from November 1, 2018 to October 31, 2019 which contained comments regarding experiences with traumatic BPI were analyzed. Posts on birth-related palsy and social content were excluded. We used inductive and deductive qualitative thematic analysis to identify recurring topics, knowledge gaps, potential intervention opportunities, and patient interaction dynamics. Two study team members coded all posts independently. Discrepancies were resolved by a qualitative research specialist.
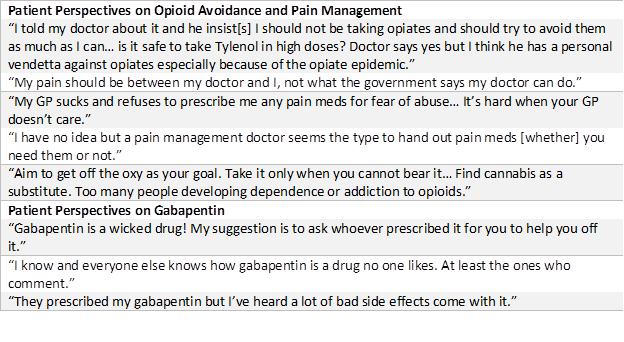
Results: Anti-opioid sentiment was a prominent recurring theme. Concern about opioid fearmongering also appeared regularly in response. Posters frequently warned of potential risks associated with opioid use. Posters referencing opioid use received responses denouncing the medications, referring to prescribers as “pill pushers”, or touting CBD oil and/or cannabis as a safer and more effective replacement. Regardless of pain described or time since initial injury, many posts heavily emphasized using positive thoughts and a “stronger” mindset instead of opioids. Such comments were often written in ways that shamed or judged others for using opioids. Some anti-opioid posters referenced each other’s comments to validate their judgments, creating the impression of confirmation bias. Also discussed were the perceived effects of the “opioid crisis” on treatment, care providers relationships, and availability of the medications. Anti-gabapentinoid sentiments were often expressed, citing adverse effects and perceived lack of efficacy.
Conclusions: These results demonstrate the prevalence of misinformation and charged opinions on neuropathic pain management, influenced in part by the “opioid epidemic” political climate, leading to broad anti-opioid sentiments and use of alternative treatments amongst patients. Gabapentinoids are viewed poorly due to adverse effects, perceived ineffectiveness, and misclassification as opioids. Analyzing BPI Facebook groups demonstrates how patient desperation for pain relief and social media access leads to an echo chamber where patients seek and share medical advice from their peers, potentially receiving information that contradicts messaging from their physicians and perpetuating a cycle of misinformation.
Back to 2021 ePosters
