Peroneal Nerve Injury: A Modern Evidence-Based Treatment Algorithm for 2021
Laura E Bashour, MS1, Helen Schafer, BS1, Umer Khan, BSc1, Derek Yan, BSA1, Carl Nunziato, MD2, Brian P Kelley, MD3, Jason M. Souza, MD4 and Brent M Egeland, MD5, (1)Dell Medical School at the University of Texas at Austin, Austin, TX, (2)University of Texas Dell Medical School, Austin, TX, (3)Dell Medical School at the University of Texas, Austin, TX, (4)Walter Reed National Military Medical Center, Bethesda, MD, (5)Section of Plastic Surgery, Dell Medical School at the University of Texas at Austin, Austin, MI
Background/Intro
Peroneal nerve injuries (PNI) can lead to weak or absent ankle dorsiflexion ("foot drop") and unsafe antalgic gait, potentially causing falls. Such injuries are difficult to address with few effective treatment guidelines available. Current guidelines lack clear treatment selection criteria given the patient's preoperative variables including demographics and injury characteristics. Treatment options include bracing, tendon transfer, nerve graft and nerve transfer. Consequently, these compound variables make management ambiguous. In this paper, we aim to evaluate the existing literature and develop an evidence-based treatment algorithm.
Materials & Methods
We conducted a systematic review of literature for keywords related to PNI and its treatment between 2000 and 2020. Each paper was evaluated for its outcomes in the context of variable presentations, patient demographics and injury timing. We included papers discussing peroneal nerve treatment approaches including these variables.
Results
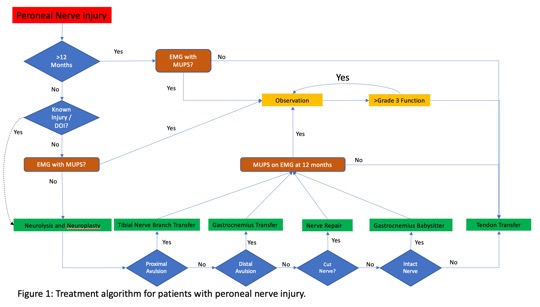
Eighteen papers, including 153 patients, met our inclusion criteria. Treatments included neuroplasty, nerve repair, nerve grafting, nerve transfers, nerve augmentation, neuromuscular transfer, free tissue transfer, and tendon transfer. The most common clinical outcome reported was ankle dorsiflexion power as graded by the Medical Research Council of Great Britain (MRC). Tendon transfer, which is the benchmark treatment for PNI, provided a consistent result with an MRC 3.9 with functional improvement at approximately 6-8 weeks. In contrast, nerve-specific treatments often reported disparate outcomes ranging from virtually no improvement to MRC >4. While tendon transfer is a purely mechanical procedure using an intact neuromuscular unit, nerve-specific approaches rely on an intermediate phase of nerve recovery which may take many months to a year. Secondarily, re-establishment of the neuromuscular unit following nerve-specific operations introduces the complexity of regeneration time, neural plasticity and sophisticated staged techniques. Based on this and the ideal reconstruction patient characteristics including age, mechanism, and timing, we developed a treatment algorithm for PNI. Specific operations will be demonstrated.
Conclusions
In this study, we develop an evidenced-based algorithm which provides updated and improved guidelines for the treatment of PNI based on patient and injury characteristics. Use of this clinical support decision tool to optimize decision-making may lead to improved patient outcomes.
Back to 2021 ePosters
