Current Trends in Brachial Plexus Surgery: Refining Indications for Exploration of the Supraclavicular Plexus
J. Ryan Hill, MD1, Steven T Lanier, MD1, Aimee S James, PhD MPH2, David M Brogan, MD, MSc2 and Christopher J. Dy, MD, MPH, FACS3, (1)Washington University, St. Louis, MO, (2)Washington University School of Medicine, St. Louis, MO, (3)Washington University in St. Louis, St. Louis, MO
Current Trends in Brachial Plexus Surgery: Refining Indications for Exploration of the Supraclavicular Plexus
Introduction: There is variability in treatment strategies for patients with brachial plexus injury (BPI). We used qualitative research methods to better understand surgeons’ rationale for treatment approaches. We hypothesized that distal nerve transfers would be preferred over exploration and nerve grafting of the brachial plexus.
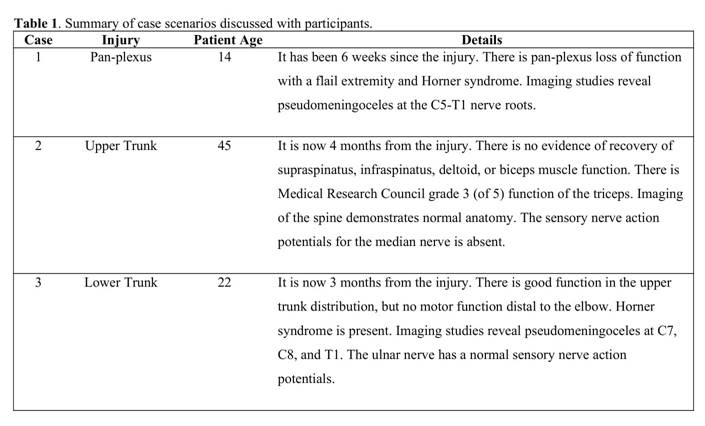
Materials & Methods: We conducted semi-structured interviews with BPI surgeons to discuss three case vignettes: pan-plexus injury, upper trunk injury, and lower trunk injury (Table 1). The interview guide included questions regarding overall treatment strategy, indications and utility of brachial plexus exploration, and role of nerve grafting and/or nerve transfers. Interview transcripts were coded by 2 researchers. We performed inductive thematic analysis to collate these codes into themes, focusing on the role of brachial plexus exploration in the treatment of BPI.
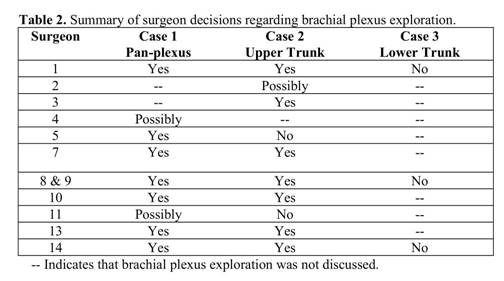
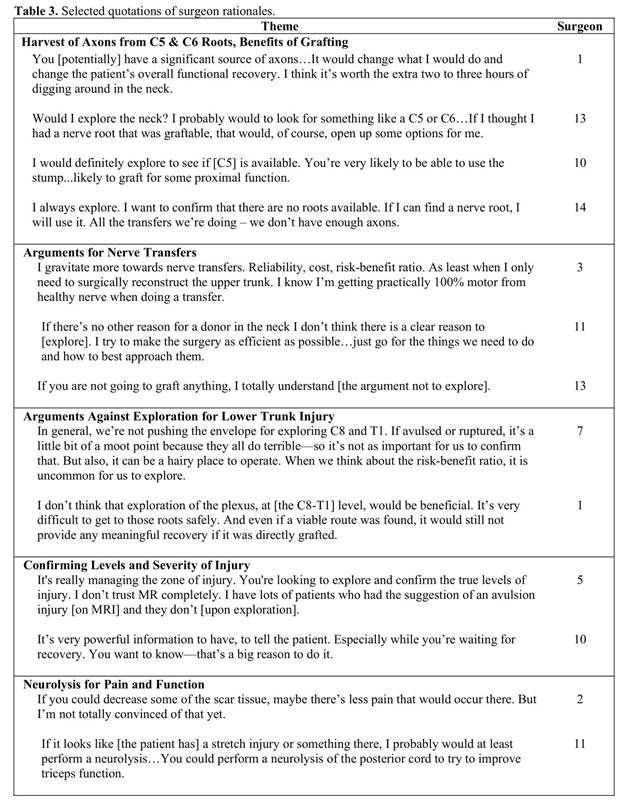
Results: A majority of surgeons (8 of 12) routinely explore the supraclavicular brachial plexus in situations of pan-plexus and upper trunk injuries. Half explore despite definitive plans for distal nerve transfers when treating pan-plexus injuries. For upper trunk injuries, two-thirds explore despite plans for nerve transfers. Decisions to explore the plexus were made based on importance of obtaining a definitive root level diagnosis, perceived availability of donor nerve roots, timing of anticipated recovery, plans for distal reconstruction, and the potential for neurolysis. Very few surgeons utilize exploration for lower trunk injuries, citing concern with technical difficulty and unfavorable risk-benefit profile (Table 2, 3).
Conclusions: Our analysis suggests that supraclavicular exploration remains a foundational component of surgical management of BPI, despite increasing utilization of distal nerve transfers. The availability of abundant donor axons and establishing an accurate diagnosis were cited as primary reasons to perform supraclavicular exploration of the brachial plexus. This analysis of surgeon interviews characterizes contemporary practices regarding the role of brachial plexus exploration in treatment of BPI.
Back to 2021 ePosters