Radial Nerve Palsy Caused by Lipoma
Matthew P Fahrenkopf, MD1, Matthew E Braza, MD1 and Steven C Naum, MD2, (1)Spectrum Health/Michigan State University, Grand Rapids, MI, (2)Orthopaedic Associates of Michigan, Grand Rapids, MI
Introduction
The majority of compressive neuropathies involve either the median or ulnar nerve. These are usually caused by known anatomic compression sites. However, a small group of patients will present with unusual symptoms or compression of a different peripheral nerve. The diagnosis and workup of this patient population can be challenging. Vague symptoms may distract physicians from the true underlying cause and physicians may pursue other etiologies. Therefore, a thorough clinical exam coupled with appropriate ancillary studies is essential to make an accurate diagnosis and treat patients in a timely manner.
Materials & Methods
A 42-year old gentleman presented to the office with a history of worsening motor weakness in the right upper extremity. He was referred from Neurosurgery, who had been pursuing a diagnosis of cervical nerve compression or thoracic outlet syndrome. No prior history of trauma, palpable mass, or recent surgery was reported. Physical examination demonstrated loss of extension to the middle, ring, and small fingers, with weakness in extension of the index finger and thumb. Wrist extension was preserved. Nerve conduction studies and electromyography were ordered. Magnetic resonance imaging was performed and identified a well-circumscribed mass over the radial head. The patient was taken back to the operating room for extirpation of the mass.
Results
Surgical exploration demonstrated encasement of the radial nerve in fibrous tissue at the level of the elbow. Dissection of the fibrous tissue from around the radial nerve, superficial sensory branch (SSBRN), and posterior interosseous nerve (PIN) demonstrated a deep seeded lipoma (Figure 1). This was noted to be compressing the aforementioned nerves with outward directed pressure. The PIN had a clinically visible narrowing from the compression (Figure 2). The lipoma was removed in its entirety while sparing the radial nerve and its branches. Complete decompression of the PIN was also performed to remove any other compression sites and facilitate nerve recovery.
Conclusions
Compressive neuropathies of the upper extremity are prevalent in the general population. Though most are caused by known anatomic compressive sites, there can be unusual etiologies. Surgeons should use their clinical exam and electrodiagnostic studies to help guide their diagnosis. Magnetic resonance imaging may be helpful to better delineate any soft tissue irregularities. Early excision, especially of lipomatous causes, may improve long-term outcomes.
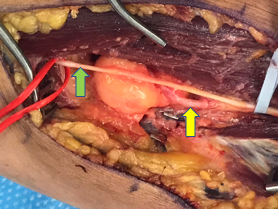
Figure 1. Lipoma under PIN (yellow) and SSBRN (green).
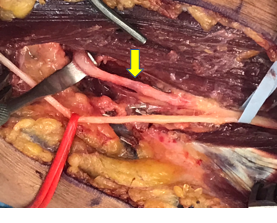
Figure 2. After lipoma excision. Note the compression of the PIN and altered color of the nerve (yellow).
Back to 2021 ePosters
