Short-term Outcomes of Novel Nerve Transfers for Shoulder External Rotation in Acute Flaccid Myelitis
Stephanie A Russo, MD, PhD, Washington University School of Medicine, St Louis, MO, Carrie Bettlach, FNP, Washington University, St. Louis, MO, Julie M West, MS, PA-C, The Ohio State University Wexner Medical Center, Columbus, OH and Amy M Moore, MD, Division of Plastic and Reconstructive Surgery, The Ohio State University Wexner Medical Center, Columbus, OH
Short-term Outcomes of Novel Nerve Transfers for Shoulder External Rotation in Acute Flaccid Myelitis
Introduction
Acute flaccid myelitis (AFM) causes flaccid paralysis following a prodromal illness primarily in children. Nerve transfers have been utilized address residual weakness for these patients. However, the unique patterns of weakness have prompted unconventional nerve transfer procedures. This study aimed to describe the novel nerve transfers used for restoration of shoulder external rotation in children with AFM and report the early outcomes.
Materials and Methods
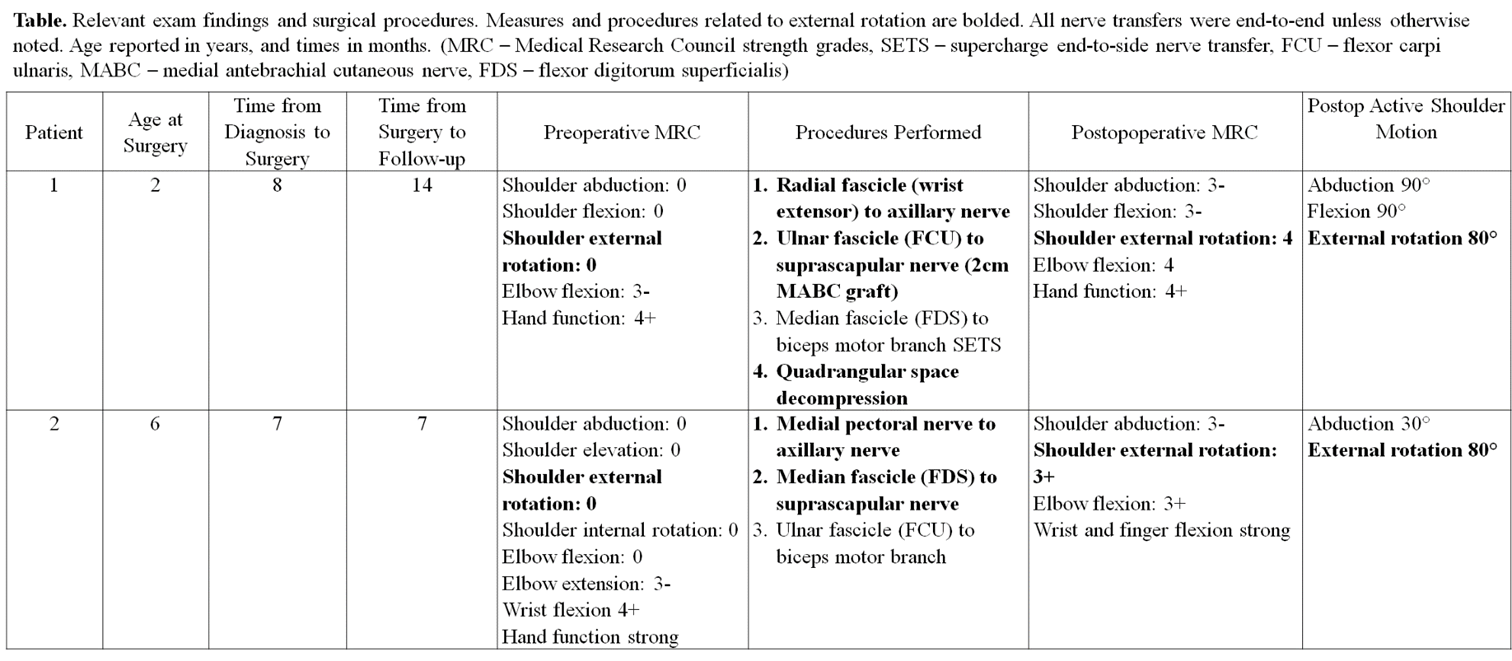
A retrospective review of two children with AFM who underwent novel transfers for shoulder external rotation was completed. Surgery was performed 7-8 months after AFM diagnosis (Table). Both patients had anterior, infraclavicular approaches that allowed access to both donor and recipient nerves. In patient 1, a primarily wrist extension radial nerve fascicle was transferred to the axillary nerve, and a primarily flexor carpi ulnaris ulnar nerve fascicle was transferred to the suprascapular nerve with a 2cm medial antebrachial cutaneous nerve autograft. In patient 2, the medial pectoral nerve was transferred to the axillary nerve, and a primarily flexor digitorum superficialis median nerve fascicle was transferred to the suprascapular nerve. The patients’ pre- and postoperative Medical Research Council (MRC) muscle strength grades and active external rotation measures were reviewed.
Results
Fourteen months after surgery, patient 1 had MRC grade 4 external rotation with 80° of active motion. Seven months after surgery, patient 2 had MRC grade 3+ external rotation with 80° of active motion. There were no donor site deficits.
Conclusions
Patients with AFM present a unique challenge as their proximal weakness and preserved distal function do not follow typical peripheral nerve or brachial plexus injury patterns. This has led to development of novel nerve transfers to restore function in these patients. The patients in this case series demonstrated remarkable recovery of external rotation postoperatively using fascicles from the proximal ulnar and median nerves. In both patients, the recipient axillary and suprascapular nerves were transected for transfer. Thus, all external rotation recovery can be attributed to the nerve transfers. It is unclear why the results in these patients surpass the improvements in external rotation that are typically anticipated after nerve transfer in other patient populations. These findings indicate that unconventional nerve transfers are feasible and can be considered for AFM patients who lack more commonly utilized nerve transfer donors.
Back to 2021 Abstracts