Outcomes in alternative posterior approach, double nerve transfer for restoration of shoulder function
Lindsay E Janes, MD, Northwestern University, Chicago, IL, Christopher S Crowe, MD, University of Washington, Seattle, WA, Nikhil D Shah, BS, Northwestern Univeristy, Chicago, IL and Jason H Ko, MD, MBA, Division of Plastic and Reconstructive Surgery, Northwestern University, Chicago, IL
Introduction:
Nerve transfer techniques for restoration of shoulder abduction have dramatically improved the function and quality of life for patients in the past 20 years. We describe a reliable approach for transfer of both the medial triceps nerve branch and thoracodorsal nerve to the axillary nerve to increase axonal input to the axillary nerve. We present a retrospective review of these patients compared to alternative common axillary nerve transfers performed by a single surgeon at two institutions as well as outcomes for end to end compared to end to side nerve transfer.
Methods:
After Institutional Review Board approval, a retrospective review of patients at two institutions was conducted. Inclusion criteria included all patients 18 and older who underwent nerve transfer surgery for improvement of shoulder function by the principle investigator, between January 1, 2010 and January 1, 2019.
Results:
24 patients that underwent nerve transfer(s) for shoulder function between December 2014 to December 2018 were identified. 6 patients were excluded due to inadequate follow up or records. Age, BMI, and medical comorbidities were not statistically different between groups.
One out of three patients who underwent spinal accessory to suprascapular and triceps branch to axillary nerve transfer achieved improvements of three MRC grades or better compared to seven out of thirteen in the triceps branch and thoracodorsal to axillary nerve transfers. All three patients who underwent triple nerve transfer (spinal accessory to suprascapular and both triceps branch and thoracodorsal to axillary nerve transfers) achieved improvements of 3 MRC grades or better
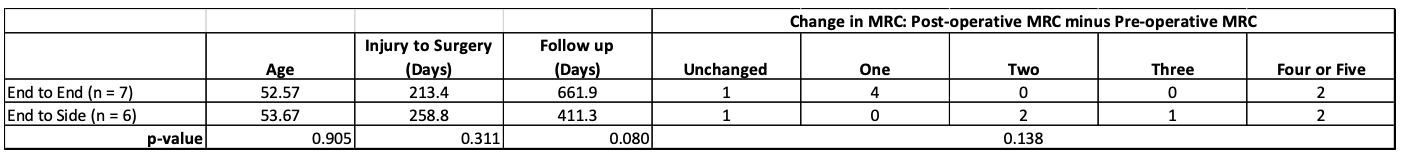
Among the patients that had R to Ax and TD to Ax transfers, there were 7 end-to-end coaptations, and 6 end-to-side coaptations. Only 28% of the end-to-end coaptations had MRC improvements of two or greater, compared with 83% of end-to-side coaptations (Table 2).
Table 1
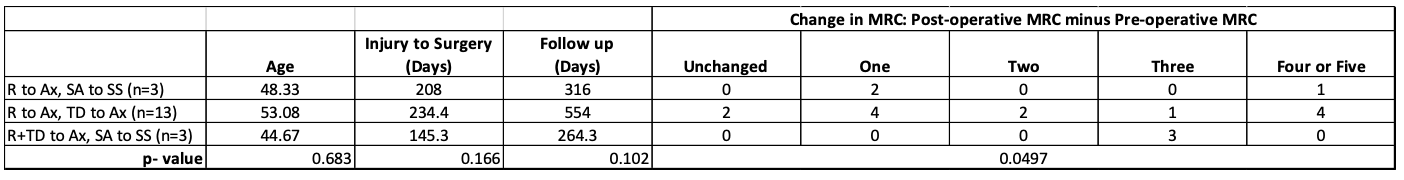
Table 2
Conclusions:
We show significant improvements in shoulder abduction by utilizing the thoracodorsal nerve to increase the axonal donation to power the axillary nerve, without the sacrifice of the spinal accessory nerve. Further, we demonstrate significant improvements with end to side coaptation when intra-operative stimulation of the axillary nerve reveals some residual function.
Back to 2021 Abstracts
