Approach to the Pan-Brachial Plexus Injury: variation in surgical strategies among surgeons
Steven T Lanier, MD1, J. Ryan Hill, MD1, Aimee S James, PhD MPH2, David M Brogan, MD, MSc2 and Christopher J. Dy, MD, MPH, FACS3, (1)Washington University, St. Louis, MO, (2)Washington University School of Medicine, St. Louis, MO, (3)Washington University in St. Louis, St. Louis, MO
Approach to the Pan-Brachial Plexus Injury: variation in surgical strategies among surgeons
Introduction: Treatment of pan-brachial plexus injuries has evolved significantly over the past two decades with the refinement and introduction of new surgical techniques, particularly free functional muscle transfer. The extent to which contemporary brachial plexus surgeons utilize various techniques as part of their treatment algorithm for pan-plexus injuries and the rationale underlying these choices remains largely unknown.
Materials and Methods: A case scenario was posed to 12 brachial plexus surgeons during semi-structured qualitative interviews. The case involved a young patient presenting 6 weeks after a pan-plexus injury from a motorcycle accident. Surgeons were asked to formulate a treatment plan. Inductive thematic analysis was used to identify commonalities and variation in approach to treatment.
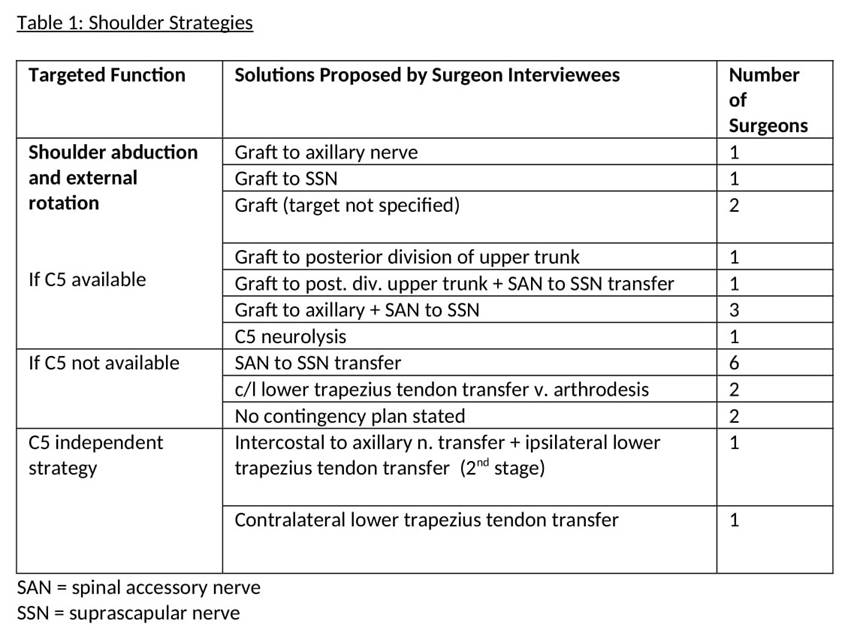
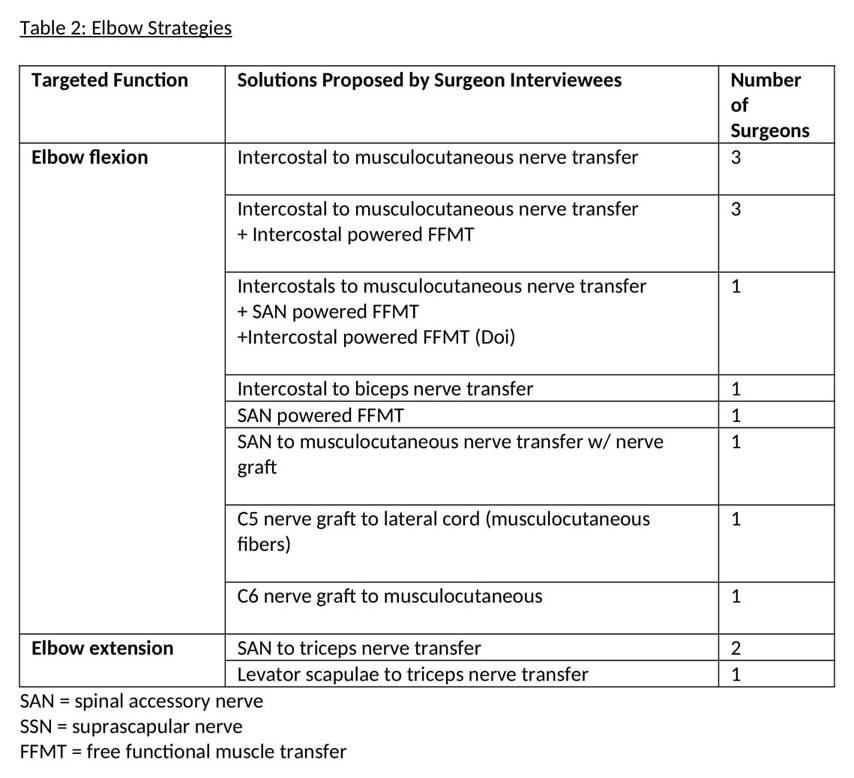
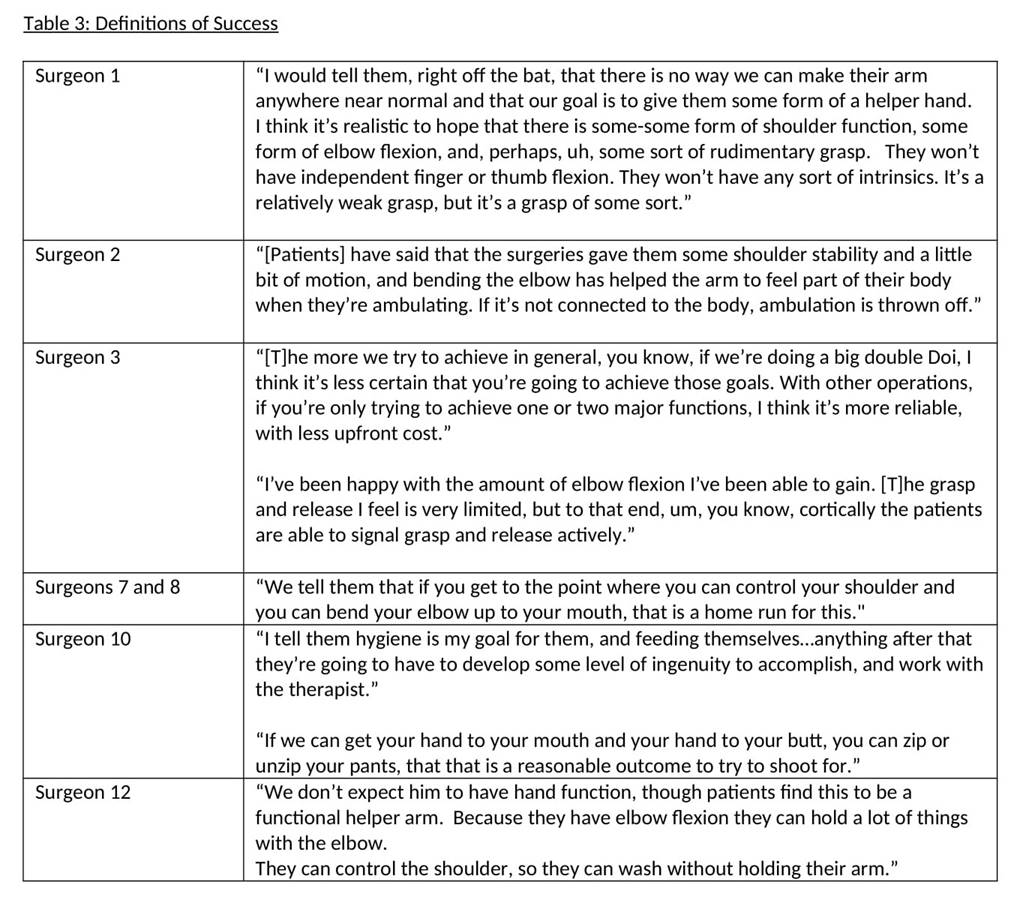
Results: For shoulder function, the majority of surgeons would graft from a viable C5 nerve root if possible though the chosen target varied (Table 1). Recipients included the suprascapular nerve (n=1), posterior division of upper trunk (n=2), and axillary nerve (n=4). Two thirds of surgeons would address elbow flexion with nerve transfers, though half would combine this with a free functional muscle transfer to increase elbow flexion strength (Table 2). Slightly over half of surgeons (7 of 12, 58%) would utilize free functional muscle transfer to restore finger flexion. Finger extension, intrinsic function, and sensation were not prioritized. Definitions of success were tempered and focused on use of the reconstructed extremity to assist with dressing, hygiene, and feeding (Table 3). The influence of mentorship, personal experience, and patient age were all factors cited to influence choice of operative strategy.
Conclusions: Our study sheds light on current trends in the approach to pan-plexus injuries in the U.S. and identifies areas of variability that would benefit from future study. The optimal shoulder target and the role for grafting to the MCN for elbow flexion merit further investigation. The role of FFMT continues to evolve, and further studies may better define the role of ICN to MCN transfer and FFMT to restore elbow flexion.
Back to 2021 Abstracts