Morbidity and function loss after resection of malignant peripheral nerve sheath tumors
Enrico Martin, MD, University Medical Center Utrecht, Utrecht, Netherlands, Courtney Pendleton, MD, Mayo Clinic, Rochester, MN, Cornelis Verhoef, MD, PhD, Erasmus Medical Center, Rotterdam, Netherlands, Robert J. Spinner, MD, Department of Physical Medicine and Rehabilitation, Mayo Clinic, Rochester, MN and J. Henk Coert, MD, PhD, Plastic-, Reconstructive- and Hand surgery, University Medical Center Utrecht, Utrecht, Netherlands
Background: Malignant peripheral nerve sheath tumors (MPNST) are aggressive soft tissue sarcomas and their resection may lead to serious morbidity. Postoperative motor and sensory deficits have earned little attention in literature and their reconstruction is infrequently carried out. This study aimed to identify the incidence and at-risk patients of postoperative motor and sensory deficits in MPNST. As well as investigating the outcomes of functional reconstructions.
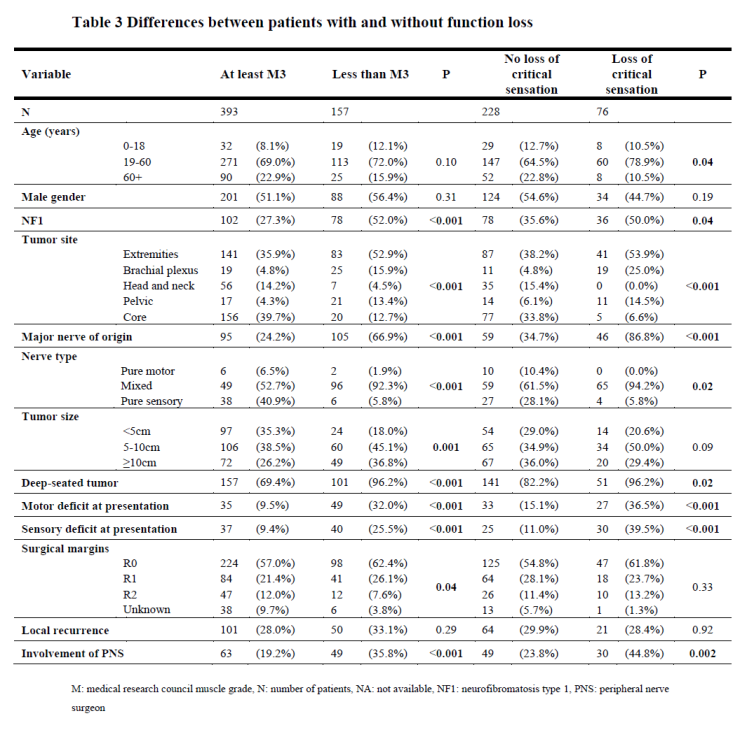
Methods: Postoperative function and treatment of MPNSTs diagnosed from 1988-2019 in 10 cancer centers was obtained. Patients with and without function loss, ≤M3 motor grade or critical sensory loss, were compared. Critical sensation was defined as partial or complete loss of hand, feet, or buttocks sensation.
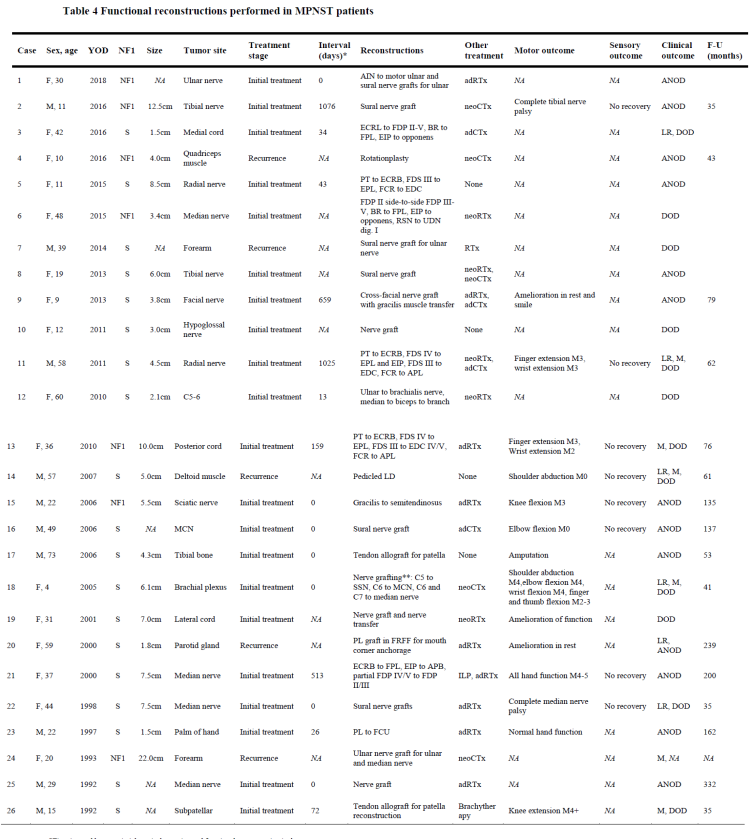
Results: Seven-hundred-fifty-six patients (33.4% neurofibromatosis type 1, NF1) were included (Table 1). MPNSTs most commonly occurred at extremity sites (37.8%) and 34.4% were known to originate from a major nerve. Of 658 surgically treated patients, 27.2% had ≤M3 muscle power and 24.3% critical sensory loss (Table 2). Amputations were carried out in 61 patients. NF1 patients, large, deep-seated, extremity, and plexus tumors originating from major nerves more commonly lead to motor and sensory loss (all p<0.05, Table 3). A total of 11 nerve grafting procedures, 4 nerve transfers, 9 tendon transfers, 3 tendon grafts, and 2 free functioning muscle transfers were performed in 26 patients (Table 4). The majority (64%) of these reconstructed patients regained at least M3 muscle power and 33% M4 despite 86% receiving multimodal therapy. Unsatisfactory results were mainly seen re-resections for recurrences or inadequate margins.
Conclusions: The resection of MPNSTs commonly resulted in major motor and sensory deficits. MPNSTs arising from major nerves, NF1 patients, large, and deep-seated tumors were at higher risk for developing postoperative morbidity. Functional reconstructions have rarely been performed, but can improve functional outcomes.

Back to 2021 Abstracts

