Lower Extremity Nerve transfers to Restore Function in Patients with Acute Flaccid Myelitis: Two-year Outcomes
Stephanie A Russo, MD, PhD, Washington University School of Medicine, St Louis, MO, Carrie Bettlach, FNP, Washington University, St. Louis, MO and Amy M Moore, MD, Division of Plastic and Reconstructive Surgery, The Ohio State University Wexner Medical Center, Columbus, OH
Lower Extremity Nerve transfers to Restore Function in Patients with Acute Flaccid Myelitis: Two-year Outcomes
Introduction
Acute flaccid myelitis (AFM) is characterized by flaccid weakness following prodromal symptoms. Patients typically have varying degrees of recovery, but persistent weakness is common. Novel nerve transfer techniques have been developed to augment lower extremity function in this population. This study aimed to assess two-year outcomes of lower extremity nerve transfers for children with AFM.
Materials and Methods
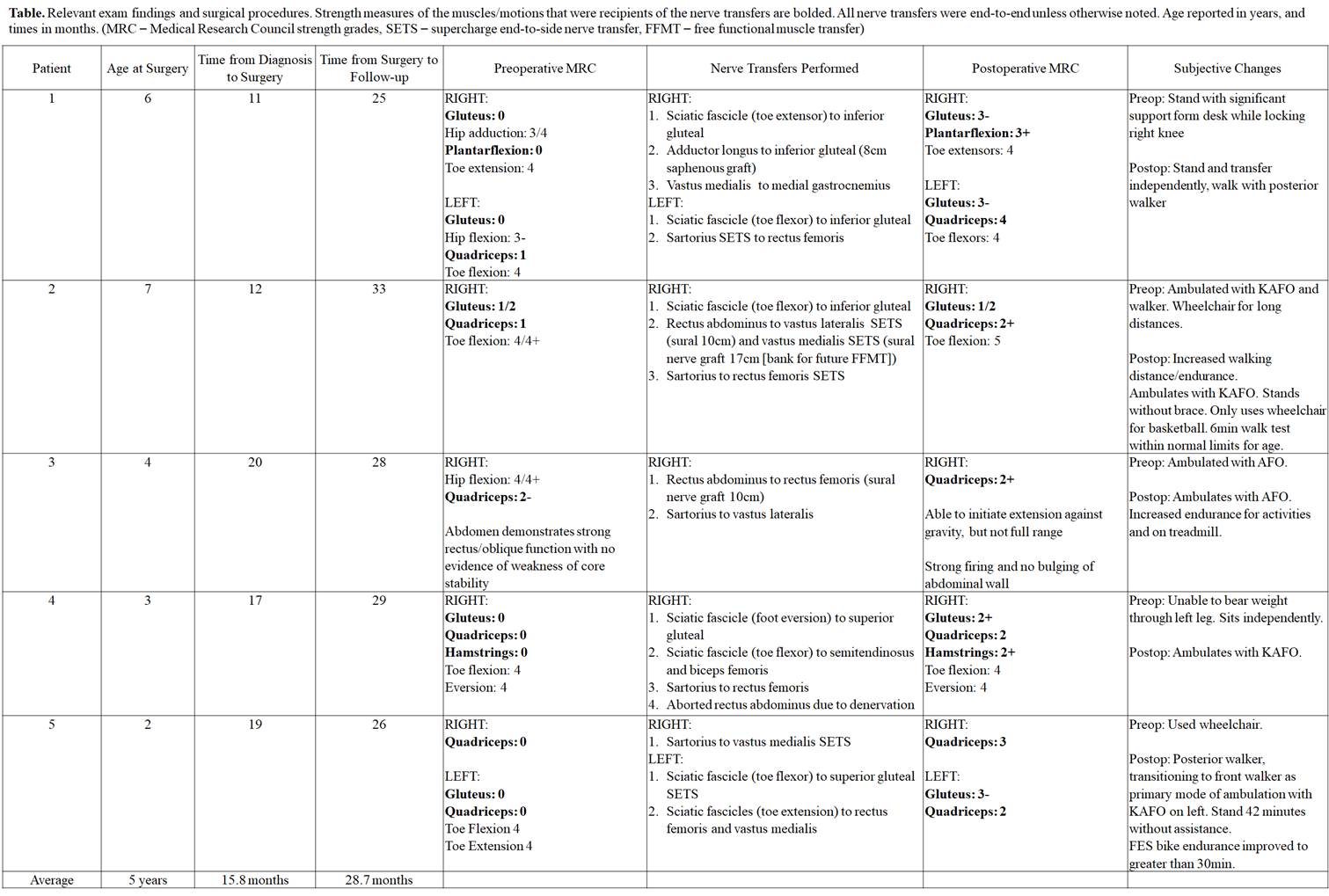
Retrospective review was performed for five children with AFM who had lower extremity nerve transfers and at least 24-month follow-up. Average age at surgery was 4.6 years, and average follow-up was 28.7 months. Nerve transfer procedures included sciatic fascicular transfers to inferior/superior gluteal, hamstring, or quadriceps motor branches; sartorius to quadriceps motor branches; rectus abdominus to quadriceps motor branches; adductor longus motor branch to inferior gluteal nerve; and vastus medialis to medial gastrocnemius motor branches (Table). Pre- and postoperative Medical Research Council (MRC) muscle strength grades were reviewed, and subjective changes in function were recorded.
Results
A variety of nerve transfers were utilized in seven limbs with average time to surgery from AFM diagnosis of 15.7 months (Table). Restoration of gluteal, femoral, hamstring, and gastrocnemius function was attempted. Variable MRC grade improvement was found (range MRC grade 0-3). All patients reported subjective improvements in function (Table). Three patients transitioned from wheelchair use to ambulation. Two patients were ambulating preoperatively, and both reported improved activity endurance postoperatively.
Conclusions
The unique needs of this patient population and variable patterns of residual weakness require meticulous assessment and development of individualized surgical plans. Establishing appropriate expectations is imperative. However, in many children, the surgical risks are low and potential benefits are monumental. While improvement in MRC grades were modest, all patients reported substantial subjective improvements in function. Notable postoperative changes were identified despite the relatively late time to surgery. With appropriate goals and expectations in mind, functional improvement, including ambulation, may be achievable.
Back to 2021 Abstracts
