The Efficacy and Safety of Different Surgical Techniques for Cubital Tunnel Decompression: A Systematic Review and Network Meta-Analysis
Ryckie George Wade, MBBS MSc MClinEd MRCS FHEA1, Timothy Thomas Griffiths, MRES2, Robert J Flather, MBChB2, Nicholas E Burr, MBBS MRes MRCP PhD2, Grainne Bourke, MB BCh BAO FRCSI FRCS(Plast)3 and Mario Teo, MBChB, BMedSci, FRCS(SN)4, (1)Department of Plastic and Reconstructive Surgery, University of Leeds, Leeds, United Kingdom, (2)University of Leeds, Leeds, United Kingdom, (3)Leeds Teaching Hospitals Trust, Leeds, United Kingdom, (4)Bristol Institute of Clinical Neuroscience, Bristol, United Kingdom
Introduction: Cubital Tunnel Syndrome (CuTS) is the 2nd most common compressive neuropathy. There are numerous different operations performed globally to treat CuTS although to-date, conventional (pairwise) meta-analyses have been unable to determine which procedure is the most effective and safe. Network meta-analysis (NMA) provides more precise estimates than standard pairwise meta-analysis and can rank interventions by efficacy, to inform clinical decisions.
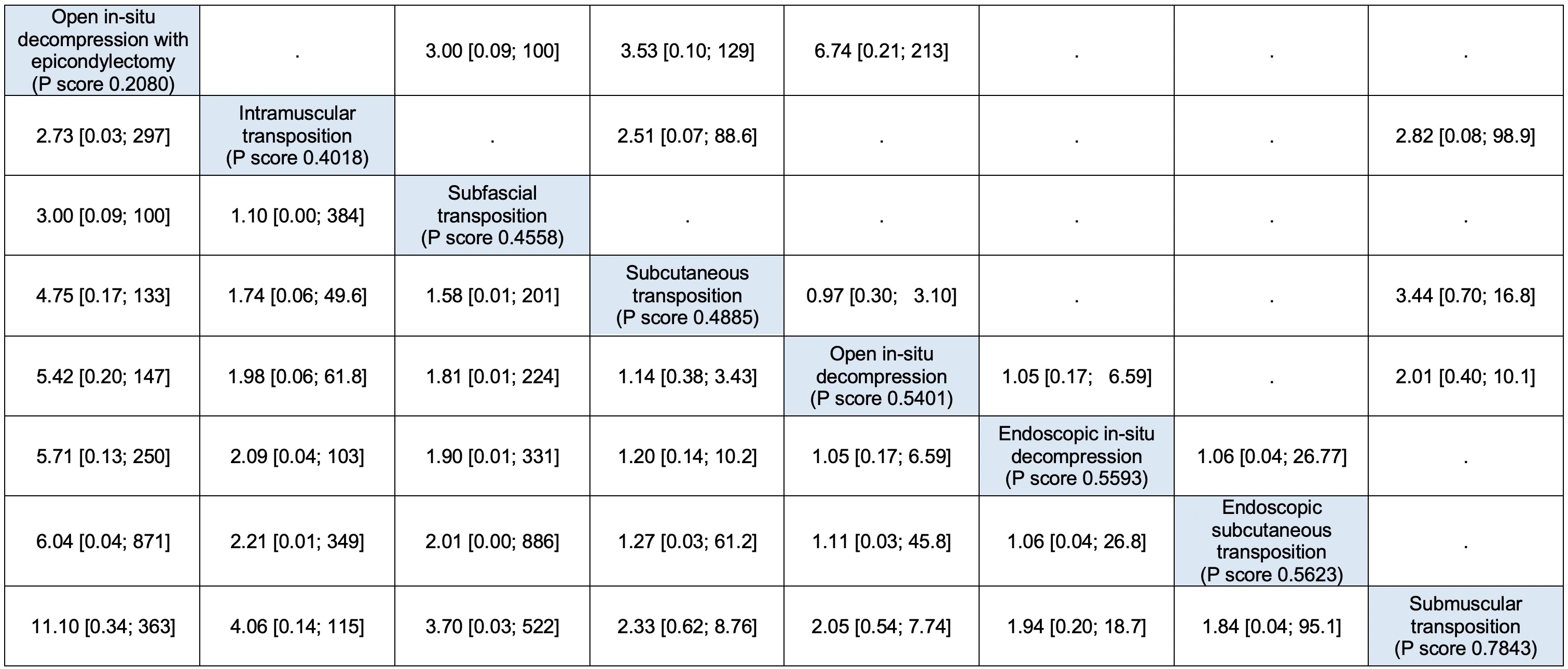
Methods: We searched PubMed, Embase and CENTRAL for studies comparing any surgical treatments for adults with primary CuTS. The primary outcome was response to treatment (i.e. symptomatic improvement). The secondary outcomes were peri-operative complications, reoperation and recurrence. We performed NMA to estimate the relative efficacy of interventions using relative risks (RR) with 95% confidence intervals (CI). Surgical techniques are ranked by their probability of being the best (P-score) and presented in league tables, with the "best" treatment in the top left and "worst" in the bottom right; a RR <1 favours the row-defining treatment.
Results: We included 31 studies of 2420 patients undergoing 8 different operations (Figure 1). Overall, 85% of patients improved with surgery; in-situ decompression was most effective (Figure 2). Postoperatively, 3% of patients developed complications and again, in-situ decompressions were least risky (Figure 3). Overall, 4% of patients required revision surgery; open in-situ decompression was associated with fewest re-operations (Figure 4). During surveillance, 5% of patients developed recurrence and open in-situ decompression with epicondylectomy had the lowest risk (Figure 5).
Conclusions: Open in-situ decompression (with or without medial epicondylectomy) appears to be the most effective and safe procedure for patients with primary CuTS.
Figure 1. Network plot of studies included in the primary analysis of response to treatment. The size of the nodes correspond to the number of patients, the thickness of the connecting lines corresponds to the number of studies and the red colour of the lines denotes the high risk of bias. NRS = non-ransomised studies, RCT = randomised controlled trias.
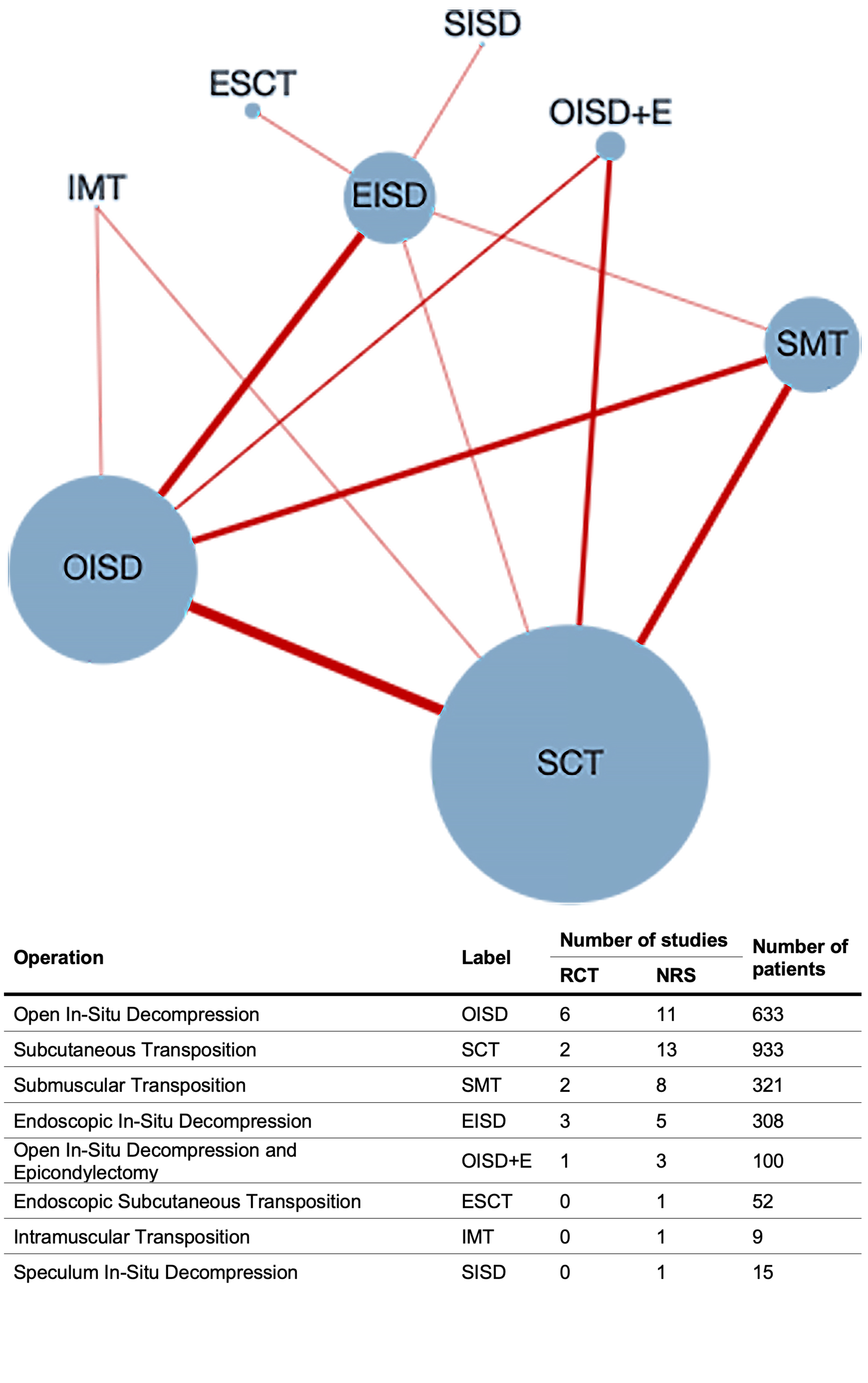
Figure 2. League table of the relative risk of responding to treatment (i.e. improving). Treatments are ranked by their chance (P score) of improving symptoms.
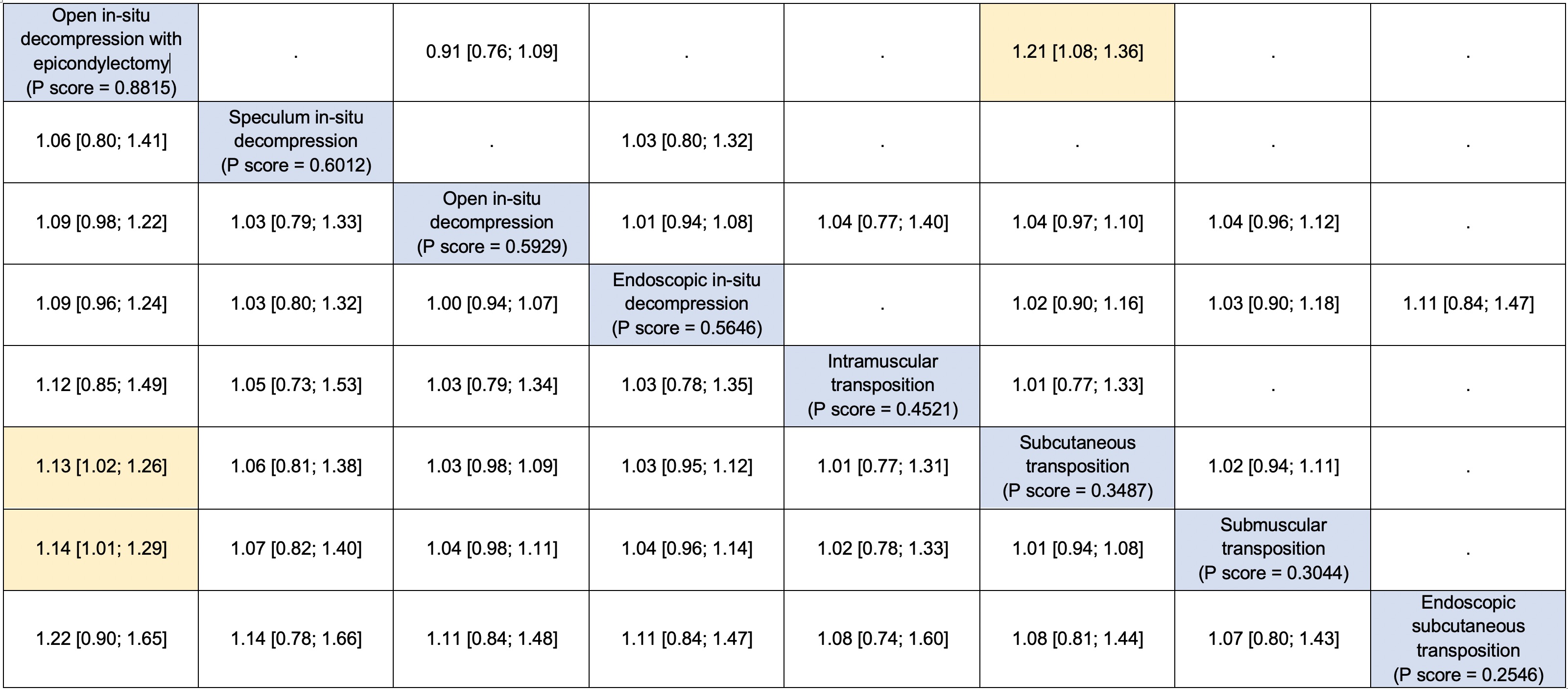
Figure 3. League table for the relative risk of complications.
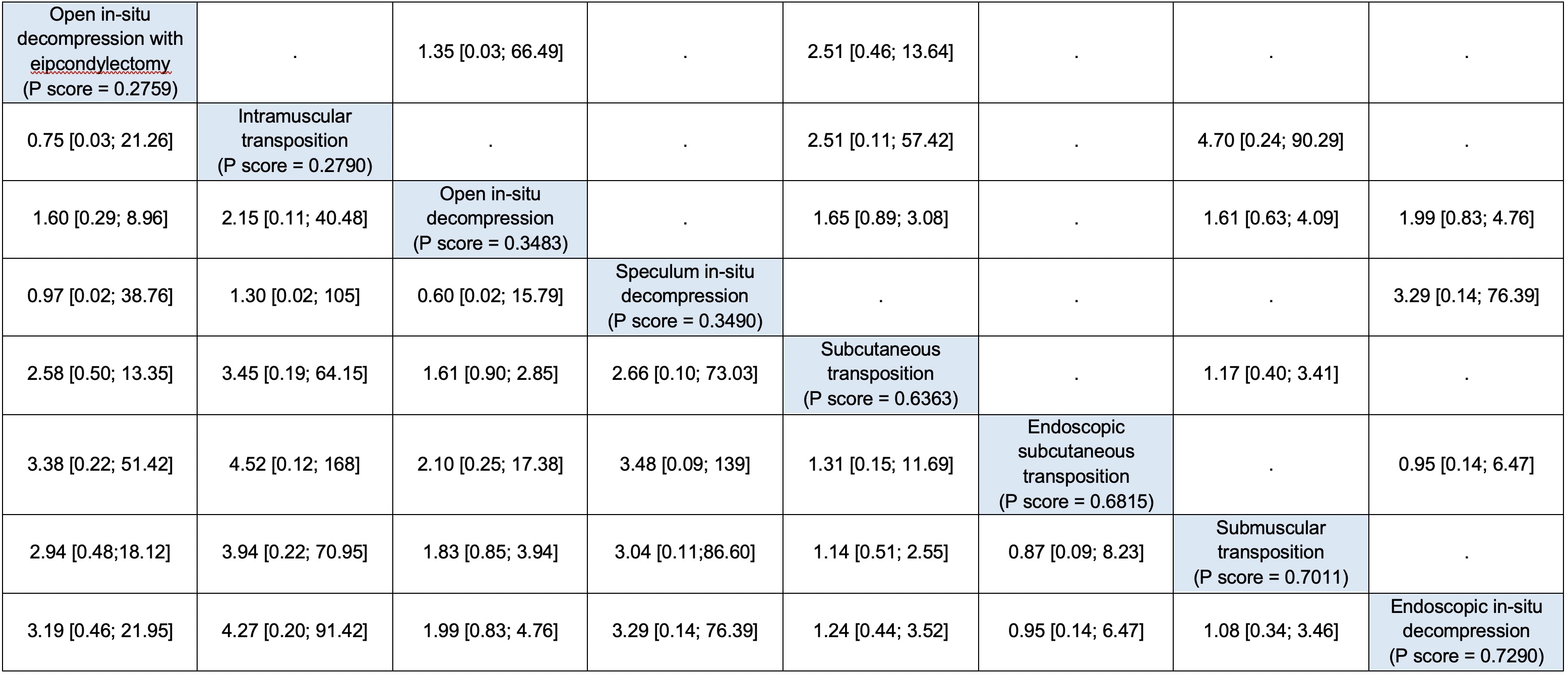
Figure 4. League table for the relative risk of reoperation.
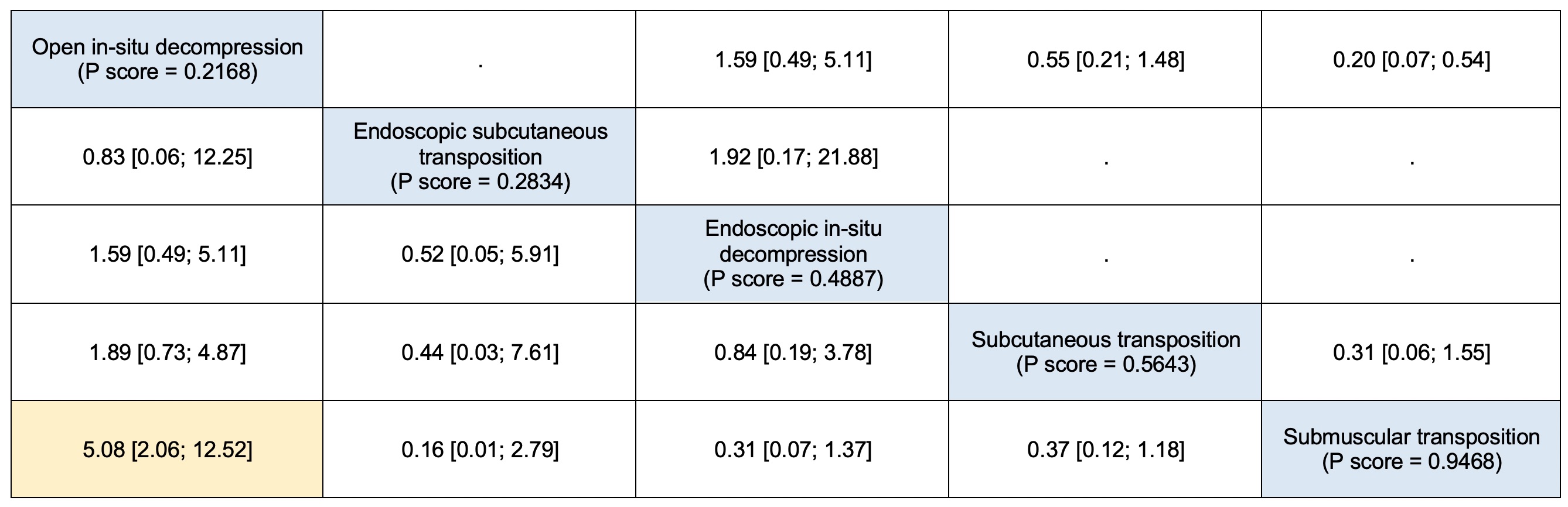
Figure 5. League table for the relative risk (with 95% confidence intervals) of recurrence.
Back to 2021 Abstracts
