Preliminary results of motor outcomes following nerve transfer and motor retraining for upper extremity paralysis caused by acute flaccid myelitis
Julie Werner, PhD, Children's Hospital of Los Angeles, Los Angeles, CA, Jordan R Wlodarczyk, MD, MS, LAC/USC Hospital, Los Angeles, CA, Graham Ives, M.D., Keck School of Medicine, Los Angeles, CA, Erin L Weber, MD, PhD, Division of Plastic and Reconstructive Surgery, University of Southern California, Los Angeles, CA and Mitchel Seruya, MD, Keck School of Medicine of the University of Southern California, Los Angeles, CA
Purpose:
Acute flaccid myelitis (AFM) is a neuromuscular disease drawing increasing awareness. No primary medical intervention exists to treat the resulting paralysis. Nerve transfer has been increasingly offered in AFM to treat previously thought to be a permanent disability. At this stage the effect of nerve transfer in AFM patients is incompletely understood. The purpose of this study is to demonstrate with timely post-paralysis nerve transfer and intensive occupational therapy robust returns in motor function can be achieved.
Methods: Chart review was completed between 3/25/2016 and 2/28/2020 evaluating motor function of patients with acute flaccid myelitis (AFM) undergoing nerve transfer followed by intensive occupational therapy. Patients with postoperative follow up less than 6 months duration and patients receiving a gracilis free flap were excluded. All patients received therapy including range of motion, electrical stimulation, EMG biofeedback, graded strengthening, and activities targeting motor planning skills and donor-recipient action coupling. Motor function was measured with the Active Movement Scale (AMS) preoperatively and postoperatively. Bivariate correlation coefficient correlated each of the following with motor recovery: age, length of follow up, and time from onset of paralysis to nerve transfer.
Results:
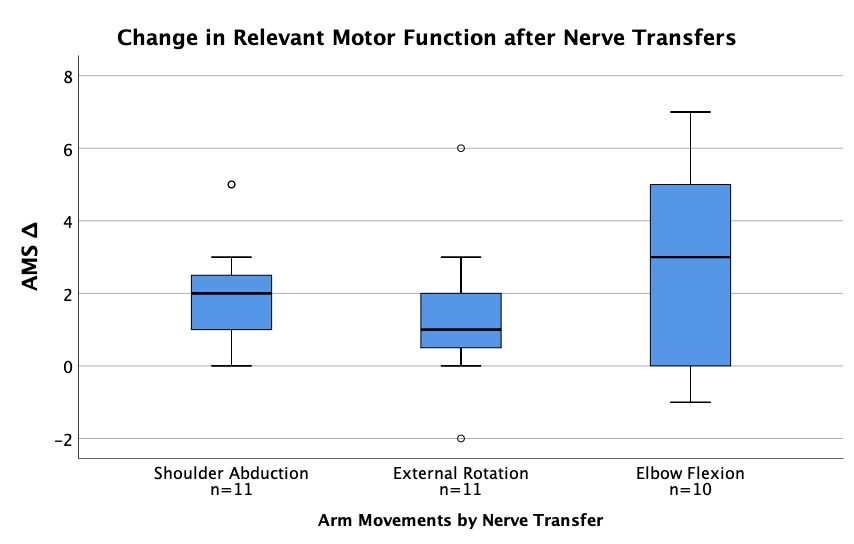
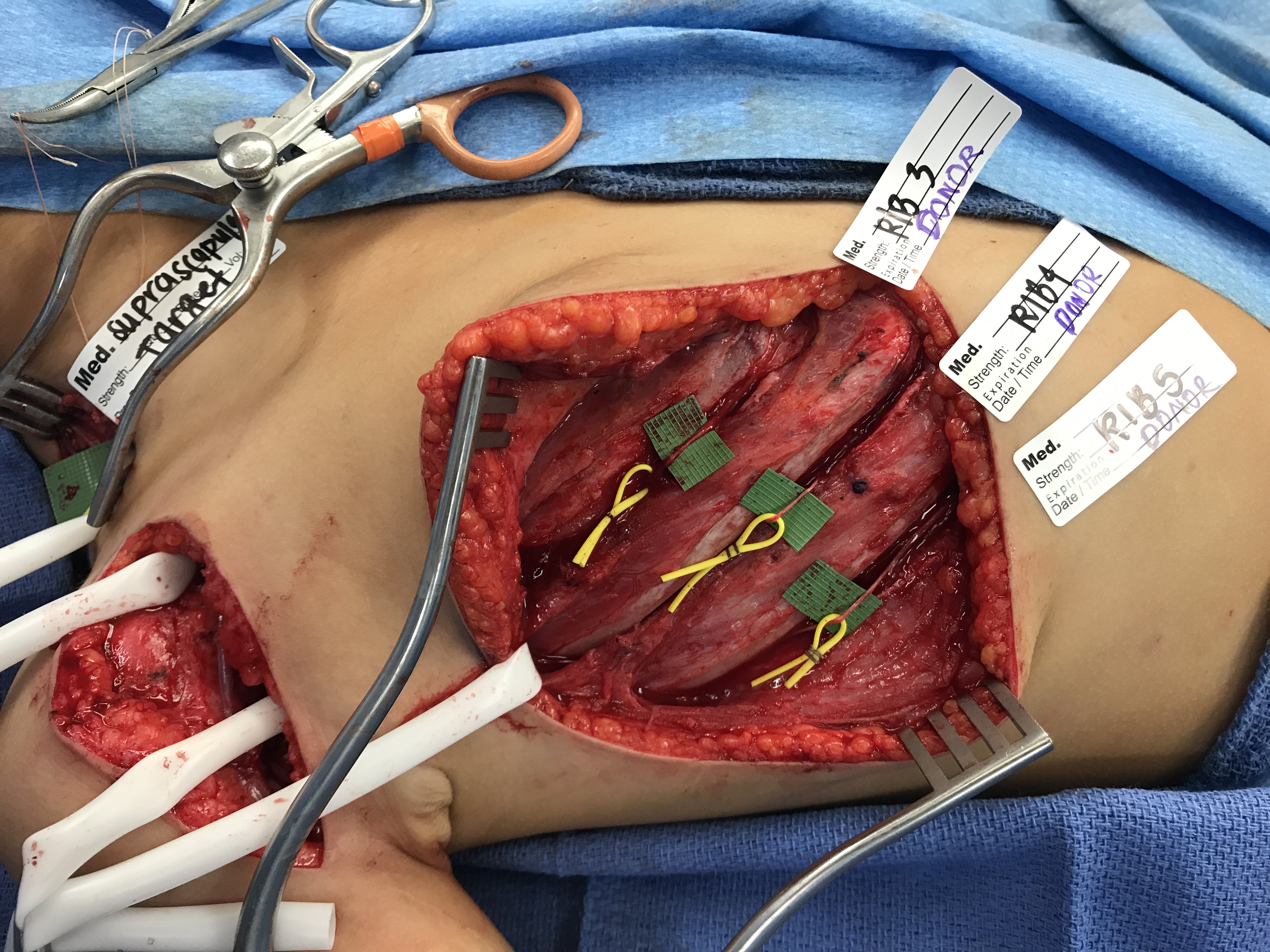
16 patients, average age 8 (±4 SD, range 2-18) years old, underwent a total of 48 nerve transfers. Mean time from paralysis to surgery was 15.1 (±7.4, 4-28) months and mean post-operative follow-up time was 16.7 (±8.6, 6-42) months. The most common donor nerves were the T3-T5 intercostals and the medial pectoral nerve. The most common targets were axillary nerve, suprascapular nerve (SSN), and musculocutaneous nerve (MCN) biceps branch. Mean AMS scores improved as follows: shoulder abduction by 2.1 (±1.6, n=10), shoulder external rotation by 1.5 (±2.0, n=11), and elbow flexion by 2.6 (±2.6, n=11), respectively. Time from onset of paralysis to nerve transfer did not correlate with motor function (spearman's coefficient 0.045, p=0.764). However, increased length of follow up at final evaluation (spearman's coefficient 0.347, p=0.016) and younger age at the time of nerve transfer (spearman's coefficient -0.294, p=0.042) correlated with greater motor recovery. Only one patient had a surgical complication, requiring admission to the PICU for tracheitis.
Conclusion:
Nerve transfer to address paralysis from AFM is a safe and efficacious and can produce significant improvements in function of targeted muscle groups. Long term outcomes must to be studied for a full understanding of the full return of function of these muscle groups.
Back to 2021 Abstracts
