Early spinal accessory-to-suprascapular nerve transfer is critical for enhanced functional outcome following traumatic brachial plexus injury.
Amir Dehdashtian, MD, MPH1, Jong-Pil Yoon, MD1, Zishen Zhuang, MS1, Shelby Svientek, MD2, Paul S Cederna, MD3 and Stephen WP Kemp, PhD1, (1)University of Michigan, Ann Arbor, MI, (2)The University of Michigan, Ann Arbor, MI, (3)Plastic Surgery, University of Michigan, Ann Arbor, MI
Introduction:
Traumatic brachial plexus injuries (TBPI) are highly debilitating and often result in life-long disability and neuropathic pain. Upper TBPI commonly leads to loss of both shoulder abduction and external rotation. Neurotization of suprascapular nerve (SSN) using spinal accessory nerve (SAN) is considered as the modality of choice to restore shoulder stability. Although nerve transfer has revolutionized the surgical management of TBPI, a consensus on the ideal time-frame to perform the surgery is currently lacking. The present study utilizes a rat model to evaluate the critical time-period to perform SAN-to-SSN nerve transfer following TBPI.
Methods:
Fifteen male Lewis rats (2-months old) were randomly assigned to one of three groups (n=5/group): (1) early surgery; (2) late surgery, or; (3) control. Following baseline behavioral assessments, all rats underwent right SSN transection. One week post-operatively, the early surgery group received SAN-to-SSN nerve transfer. A similar repair was conducted for the late surgery group after six weeks, while the control group did not receive any further nerve repair. Weekly behavioral assessments, including walking track and cylinder test, were performed serially for twelve weeks. The cylinder test was used to measure the ratio of using each front-paw to hold on the wall when rats were placed in a transparent cylinder for five minutes. Walking track analysis measured several variables such as front-paw width, length, toe spreading, and the distance between two consecutive steps. At the endpoint, compound muscle action potential (CMAP) and the latency following SSN stimulation were measured for bilateral supraspinatus muscles, and muscles were harvested and weighed. Muscle denervation atrophy was assessed using Oil-Red-O staining (detects lipofuscin) and collagen-I immunostaining. Nerve regeneration capacity was evaluated through histomorphometric analysis.
Results:
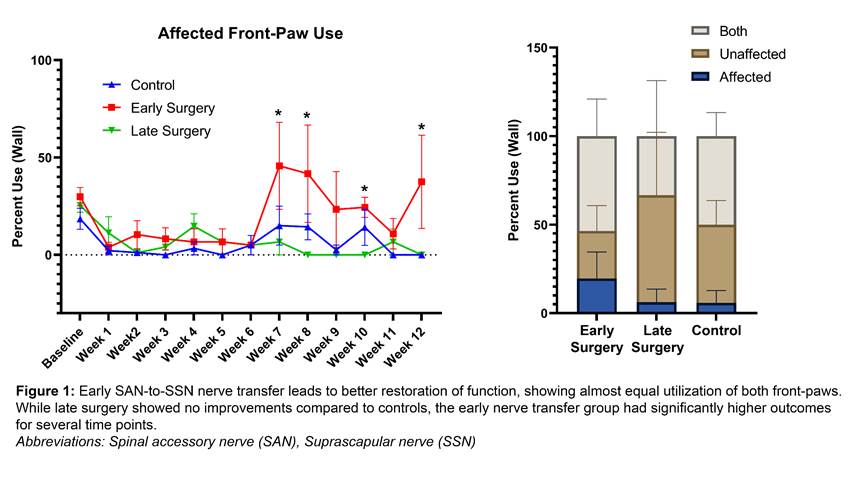
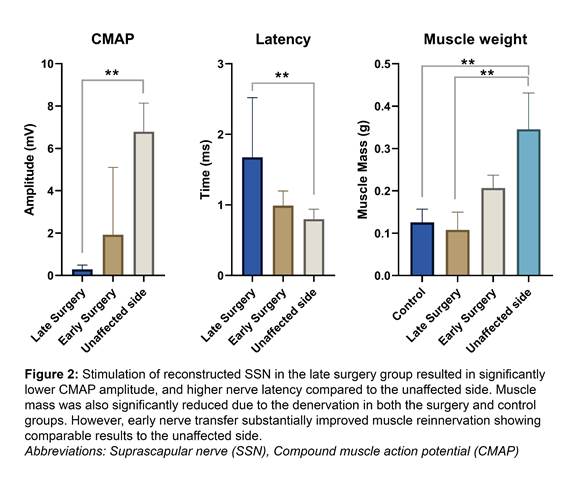
Our results showed that early SAN-to-SSN nerve transfer resulted in significantly higher utilization of the impaired front-paw compared to both the late surgery and control groups over 12 weeks (Figure 1). CMAP amplitude, latency, and muscle weight were comparable between the injured and the intact front-paws for the early surgery group only (Figure 2).
Conclusion:
Early intervention following TBPI substantially improves functional outcomes, whereas surgical delay results in loss of the optimum regenerative window.
Back to 2021 Abstracts
