Interstitial cystitis/bladder pain syndrome as referred pain from injured T12/L1 nerves: symptomatic improvement with resection of ilioinguinal and iliohypogastric nerves
Akash Chandawarkar, MD1, Kelly T Harris, MD1, Amin Herati, MD1 and A. Lee Dellon, MD, PhD2, (1)Johns Hopkins, Baltimore, MD, (2)Johns Hopkins School of Medicine Division of Plastic Surgery, Dellon Institute for Peripheral Nerve Surgery, Towson, MD
INTRODUCTION:
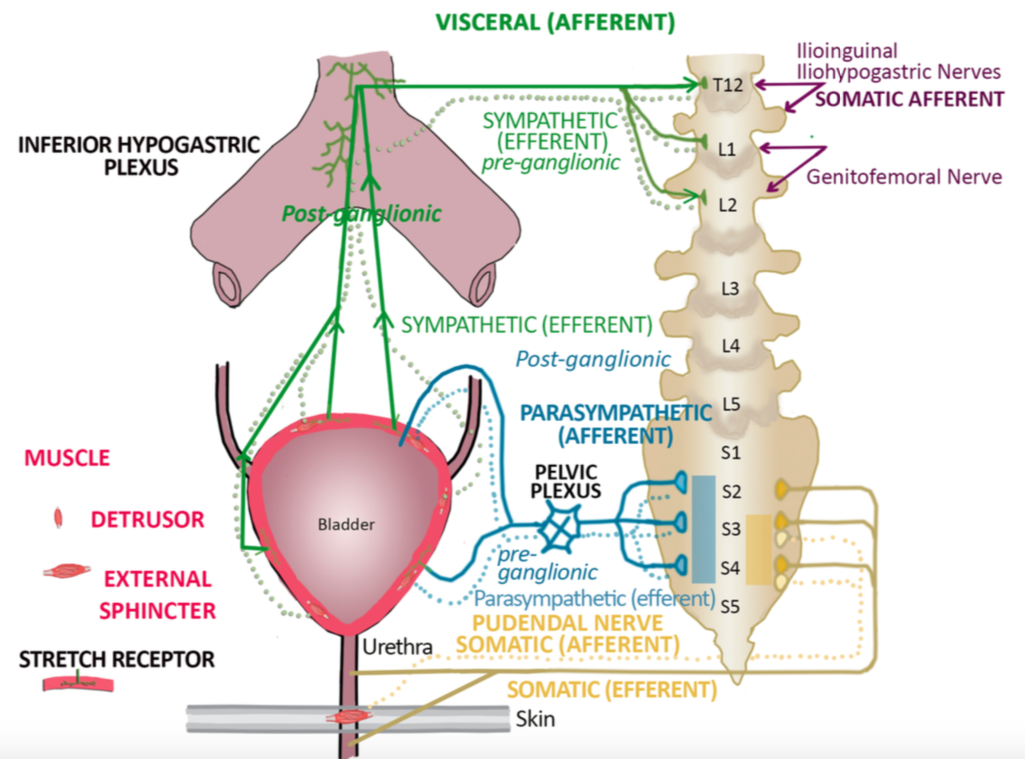
Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) remains a diagnostic and management problem for urologists and gynecologists. Ilioinguinal (II) and iliohypogastric (IH) nerves can be injured during abdominal wall surgery leaving some patients with postoperative IC/BPS. Since the II and IH nerves originate from T12 and L1 nerve roots, and sympathetic nerves to the pelvis originate from T12 and L1 (Figure 1), it was hypothesized that afferent pain signals from cutaneous injured II and IH nerves might be interpreted cortically as visceral pain from afferents traveling with sympathetic nerves, thereby creating the referred complaint of “bladder pain.”
METHODS & MATERIALS:
A prospective, IRB-approved, cohort study was undertaken with inclusion criteria of 1) presence of IC/BPS for more than one year with negative cystoscopy, negative urine cultures, and failure to respond to 6 months of medical treatment, 2) history of abdominal wall surgery, 3) presence of pain at surgical sites, 3) relief of IC/BPS with magnetic resonance (MR) guided nerve block at T12/L1. Both males and females were included. Each patient underwent resection of II and IH, unilaterally or bilaterally, based on physical findings. Outcome measures were validated O'Leary/Sant Voiding and Pain Indices (O/S) and Pelvic Pain & Urgency/Frequency Symptom Scale (PU). These were obtained pre-operatively and post-operatively.
RESULTS:
Six patients were accrued between 2015 through 2019 (two males and four females) with mean age of 52 + 19.4. Four had bilateral symptoms, two had left sided symptoms only. Mean pre-operative O/S score was 10.4 + 4.3 and PU score was 18.6 + 6.9. The follow-up time for this cohort of patients ranged from one to ten months. There was significant improvement in the O/S score (p=0.032) and in the PU score (p=0.040). There were no complications from the surgery.
CONCLUSION:
IC/BPS can exist related to referred pain from injury to cutaneous innervation of the abdominal wall supplied by the ilioinguinal and iliohypogastric nerves. This pain syndrome can be relieved by resection of these nerves.
Figure 1. Innervation of the urinary system
Back to 2020 ePosters