Variability in Surgeons' Knowledge of Recovery Barriers for Patients after Brachial Plexus Injury
Christopher Dy, MD MPH FACS1, David M Brogan, MD, MSc1, Wilson Z Ray, MD1, Liz Rolf, BS1, Anna Van Voorhis, OT, CHT1, Scott W Wolfe, MD2 and Aimee S James, PhD MPH1, (1)Washington University School of Medicine, St. Louis, MO, (2)Hand and Upper Extremity Service, Hospital for Special Surgery, New York, NY
INTRODUCTION: Increasing emphasis has been placed on multidisciplinary care for patients recovering from traumatic brachial plexus injury (BPI), with a growing appreciation for the impact of psychological and emotional components of recovery. Given that surgeons are typically charged with leading the recovery process after BPI, our objective was to build a greater understanding of how surgeons approach patients’ experiences and what types of barriers exist for patients during recovery.
MATERIALS AND METHODS: We conducted semi-structured qualitative interviews with 14 surgeons with expertise in BPI reconstruction. The interview guide contained questions regarding the surgeon’s practice and care team structure, how treatment plans and priorities are developed, barriers to recovery their patients face, and any steps surgeons take to identify or address those barriers. We used inductive thematic analysis to identify themes.
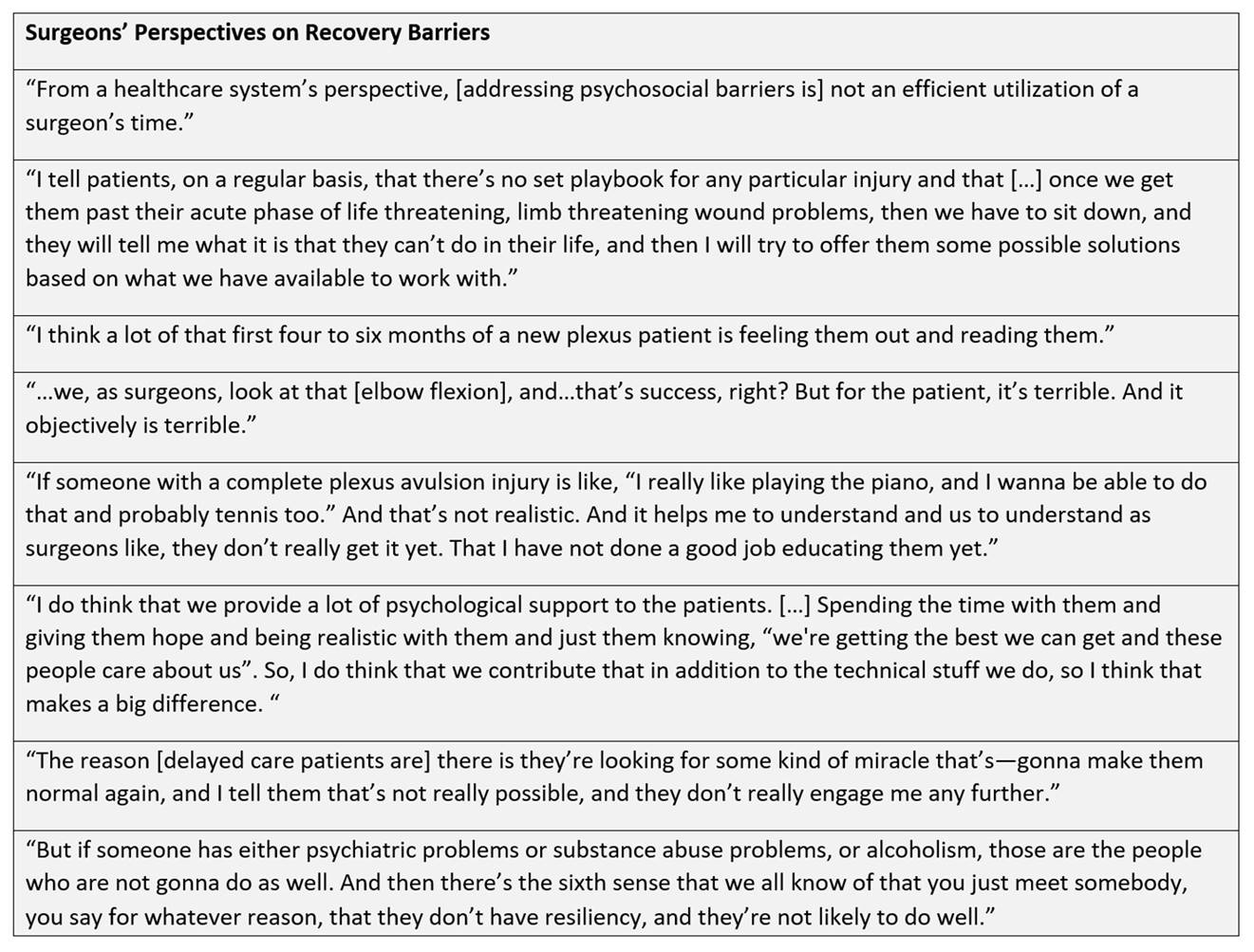
RESULTS: There was a high degree of variability in how surgeons described barriers to care for their patients. Some discussed in-depth patient histories and detailed many ways in which their patients’ recoveries and quality of life were impacted, positively or negatively, by factors including the patient’s social connections, knowledge of injury, and mental well-being. Of those surgeons aware of such “nonsurgical” barriers, some discussed how they incorporated that knowledge into their approach to treatment, whether by continuing to have such discussions with patients themselves or by building a patient care team that included staff to focus on these matters. Other surgeons described less awareness of how patients’ qualitative traits may impact their outcomes, though the potential for those traits to impact recovery outcomes was often acknowledged. Surgeons who noticed such a knowledge gap expressed uncertainty of how they might learn more, or how they might go about addressing those traits with their patients.
CONCLUSIONS: Our results demonstrate a wide variety of both awareness of and approach to addressing emotional, psychological, and social barriers to recovery for BPI patients. Further discussion with BPI surgeons can lead to identification of replicable best practices. This can set the stage for prospective evaluation of the impact that these practices may have on patient-reported outcomes and satisfaction after BPI.
FIGURE
Back to 2020 ePosters