“Being a patient the rest of my life” - The Influence of Patient Engagement on Recovery after Traumatic Brachial Plexus Injury
Christopher Dy, MD MPH FACS1, David M Brogan, MD, MSc1, Wilson Z Ray, MD1, Liz Rolf, BS1, Anna Van Voorhis, OT, CHT1, Scott W Wolfe, MD2 and Aimee S James, PhD MPH1, (1)Washington University School of Medicine, St. Louis, MO, (2)Hand and Upper Extremity Service, Hospital for Special Surgery, New York, NY
INTRODUCTION: Assessment of outcomes after adult traumatic brachial plexus injury (BPI) has historically focused on surgeon-graded measures of muscle recovery. Increasing attention is being directed to patient-reported outcomes and the patient experience after BPI. Our objective was to better understand the recovery course after surgical reconstruction for BPI, with a particular emphasis on identifying common points of frustration for patients.
MATERIALS AND METHODS: We conducted semi-structured qualitative interviews with 10 BPI patients who were 6+ months after surgical reconstruction. The interview guide contained questions regarding patients’ experience with their BPI, from the initial injury to their interview date. Inductive thematic analysis was used for the qualitative data to identify themes and knowledge gaps.
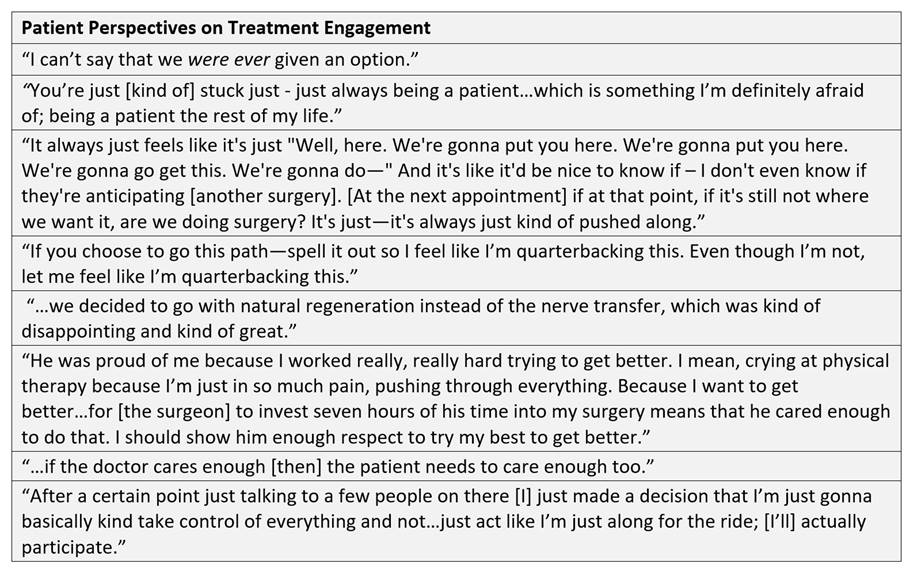
RESULTS: Patients described highly variable degrees of engagement during the course of their treatment. Many expressed frustrations related to waiting: waiting to find out what happened to them, waiting to see a new surgeon, waiting to see if the most recent surgery had any effect, or simply waiting to see if they would regain the functional ability to participate in the parts of their lives that may have been put on hold. Patients who described feeling as though they were included in the decision-making process regarding functional priorities and treatment options, seemed to be more likely to be actively engaged in and more compliant with their treatment plans. While more engaged patients still discussed waiting, they seemed to better comprehend the need for time to allow their bodies to recover and expressed less anger about their capabilities and quality of life during the recovery process.
CONCLUSIONS: Patients who feel engaged in the decision-making process were more likely to be compliant with their post-op orders and long-term care, particularly in their utilization of physical therapy, pain management, and mental health services. When coordinating multidisciplinary care, measures to encourage patients to feel agency over their outcome can bolster treatment outcomes. Based on our findings, we believe that these steps will help patients develop the self-management tools necessary to navigate the lengthy recovery process after surgical reconstruction for BPI.
FIGURE
Back to 2020 ePosters