What Are the Key Contributors to Patient Satisfaction after Traumatic Brachial Plexus Injury?
Christopher Dy, MD MPH FACS1, David M Brogan, MD, MSc1, Wilson Z Ray, MD1, Liz Rolf, BS1, Anna Van Voorhis, OT, CHT1, Scott W Wolfe, MD2 and Aimee S James, PhD MPH1, (1)Washington University School of Medicine, St. Louis, MO, (2)Hand and Upper Extremity Service, Hospital for Special Surgery, New York, NY
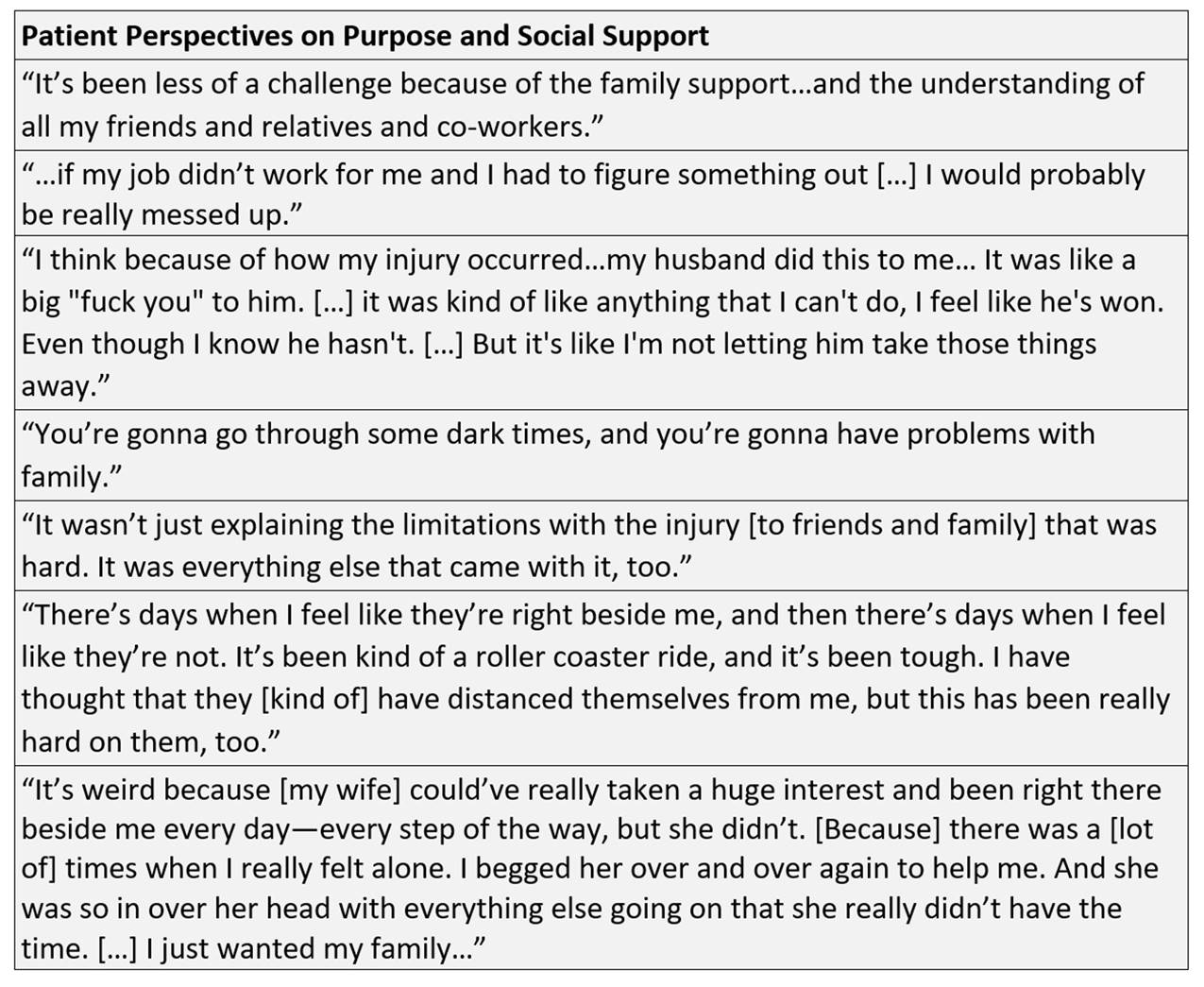
INTRODUCTION: Satisfaction and treatment outcomes after traumatic brachial plexus injury (BPI) patients varies tremendously. While much of this variation may be related to the severity of injury and available functional reconstruction options, one common thread among BPI patients is the psychological impact of the condition. These aspects of recovery can affect patient satisfaction, influence adherence with postoperative therapy, and impact willingness to endure a prolonged reconstructive process. Our objective was to understand which patient-related factors contribute to patient-reported satisfaction after BPI, with a particular interest in the role of social support and sense of purpose.
MATERIALS AND METHODS: Qualitative interviews were conducted with 10 BPI patients who were 6+ months after reconstructive surgery. The interview guide contained questions regarding patients’ BPI experience BPI, from the initial injury up to the interview. Inductive thematic analysis was used to identify themes and knowledge gaps.
RESULTS: Patients spent a great deal of time discussing who they were before their injury, and how their lives have changed since. Patients described varying levels of a sense of purpose during and after recovery. These levels were largely independent of the degree of function gained from surgery. Patients with close connections to family or friends, supportive employers, or treasured hobbies were more likely to positively describe their BPI care experience and feel satisfied with their progress, regardless of degree of functional recovery. Patients who lost careers, felt disconnected from friends or the wider world, or felt abandoned by family expressed higher dissatisfaction with their care and their recovery. Some patients with notable levels of grief and a sense of alienation from their former social circle seemed less engaged in their healthcare, and displayed higher rates of treatment noncompliance.
CONCLUSIONS: How patients perceive their BPI treatment and recovery varies widely, and is not directly linked to their functional outcome. Patients with stronger social circles and activities that give them a sense of fulfillment were more likely to be satisfied with their current status and were more likely to comply with ongoing treatment recommendations. Evaluating a patient’s social network, goals, and potential supportive adaptations early in the treatment timeline through coordinated multidisciplinary care may improve treatment compliance and subsequent satisfaction. Our work indicates that this can lead to more positive patient outcomes and a greater sense of mental well-being.
Back to 2020 ePosters