Surgical Management of Upper Extremity Nerve Injuries presenting with Painful Neuroma: Reconstructive Options with Processed Nerve Allograft
Sonu Jain, MD1, Ian Valerio, MD2, Fraser J. Leversedge, MD3, John Ingari, MD4, Bauback Safa, MD, FACS5, Timothy Niacaris, MD, PhD6, Renata Weber, MD7, Jozef Zoldos, MD8, Mihir J. Desai, MD9, Wesley P. Thayer, MD, PhD10 and Gregory M Buncke, MD5, (1)Department of Plastic Surgery, Ohio State University, Columbus, OH, (2)The Ohio State University, Columbus, OH, (3)Department of Orthopaedic Surgery, DUKE UNIVERSITY, Durham, NC, (4)Johns Hopkins Hospital, Baltimore, MD, (5)The Buncke Clinic, California Pacific Medical Center, San Francisco, CA, (6)Department of Orthopaedic Surgery, JPS Health Network, Fort Worth, TX, (7)Institute for Nerve, Hand and Reconstructive Surgery, Rutherford, NJ, (8)Arizona Center for Hand Surgery, Phoenix, AZ, (9)Vanderbilt Orthopaedics, Nashville, TN, (10)Department of Plastic Surgery, Vanderbilt University, Nashville, TN
Introduction
Management of a painful neuroma, caused by untreated injury, failed repair, and/or iatrogenic injury, remains challenging. Neuromas, which form from aberrant, uncontrolled axonal regeneration, often contribute to pain and functional impairment. Traditional methods to surgically treat the neuroma involve resection followed by strategies such as traction neurectomy, burying the proximal nerve stump into muscle or bone, capping the nerve end, or targeted muscle reinnervation (TMR). Traction neurectomy has the highest rate of neuroma recurrence and in other strategies while possibly alleviating painful symptoms, the resulting loss of nerve continuity to the distal stump causes an associated loss of neurologic function. We examined outcomes following neuroma resection with intercalary nerve reconstruction with processed nerve allograft (PNA).
Methods and Materials
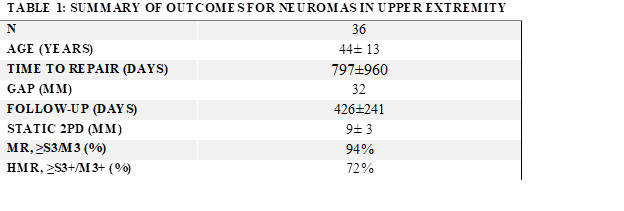
The RANGER® Study is a multicenter IRB-approved registry designed to collect data on processed nerve allografts (Avance® Nerve Graft, AxoGen, Inc). The registry database was queried for subjects presenting with painful neuromas in the upper extremity (UE) that were reconstructed with PNA and completed quantitative follow up. Demographics, nerve injury/repair, assessments, and safety were evaluated. Meaningful recovery was defined as ≥ S3/M3 on the MRC scale.
Results:
The cohort consisted of 36 painful neuromas in 26 subjects. Causation included: iatrogenic injury (14%), failed nerve repair (50%), and untreated nerve injury (36%). Anatomic distribution included: 20 digital nerves, 10 UE sensory, and 6 UE mixed sensorimotor. The mean patient age was 44±13 years and mean time-to-repair from original injury was 797±960 days. Mean gap length was 32±12mm. Mean post-reconstruction follow-up was 426±241days. Improvement in symptoms was reported in all repairs. Return to meaningful function was reported in 94% of repairs. The mean static 2PD was 9 ±3mm. No related adverse events were reported.
Conclusions
Treatment of painful neuromas with resection and intercalary PNA reconstruction is safe, successfully improved symptoms and provided meaningful functional recovery in 94% of repairs. These outcomes compare favorably to historical data for this condition. Limitations of this study include the observational study design and lack of active controls. Treatment of symptomatic neuromas using PNA is a reasonable method and should be considered in patients with chronic, symptomatic neuromas who have failed conservative treatment. This reconstruction technique provided both an opportunity to reduce pain and, unlike other approaches, restore function by reestablishing nerve continuity.
Back to 2020 Abstracts