Influence of Knowledge and Expectations on the Patient Experience during Recovery from Traumatic Brachial Plexus Injury
Christopher Dy, MD MPH FACS1, David M Brogan, MD, MSc1, Liz Rolf, BS1, Wilson Z Ray, MD1, Anna Van Voorhis, OT, CHT1, Sarah Buday, PhD2, Scott W Wolfe, MD3 and Aimee S James, PhD MPH1, (1)Washington University School of Medicine, St. Louis, MO, (2)Washington University, St. Louis, MO, (3)Hand and Upper Extremity Service, Hospital for Special Surgery, New York, NY
INTRODUCTION: Treatment outcomes and quality of life for traumatic brachial plexus injury (BPI) patients vary widely. These outcomes have not been shown to depend strictly on severity of the injury, extent of surgical treatment, or other easily quantifiable measure. Our objective was to build a greater understanding of each patient’s experiences in order to identify common qualitative factors and themes in patients’ lives that affect outcomes.
MATERIALS AND METHODS: Qualitative interviews were conducted with 10 BPI patients who were 6+ months after reconstructive surgery. The interview guide contained questions regarding patients’ experience with their BPI, from the initial injury to the interview date. Inductive thematic analysis was used for the qualitative data to identify themes and knowledge gaps.
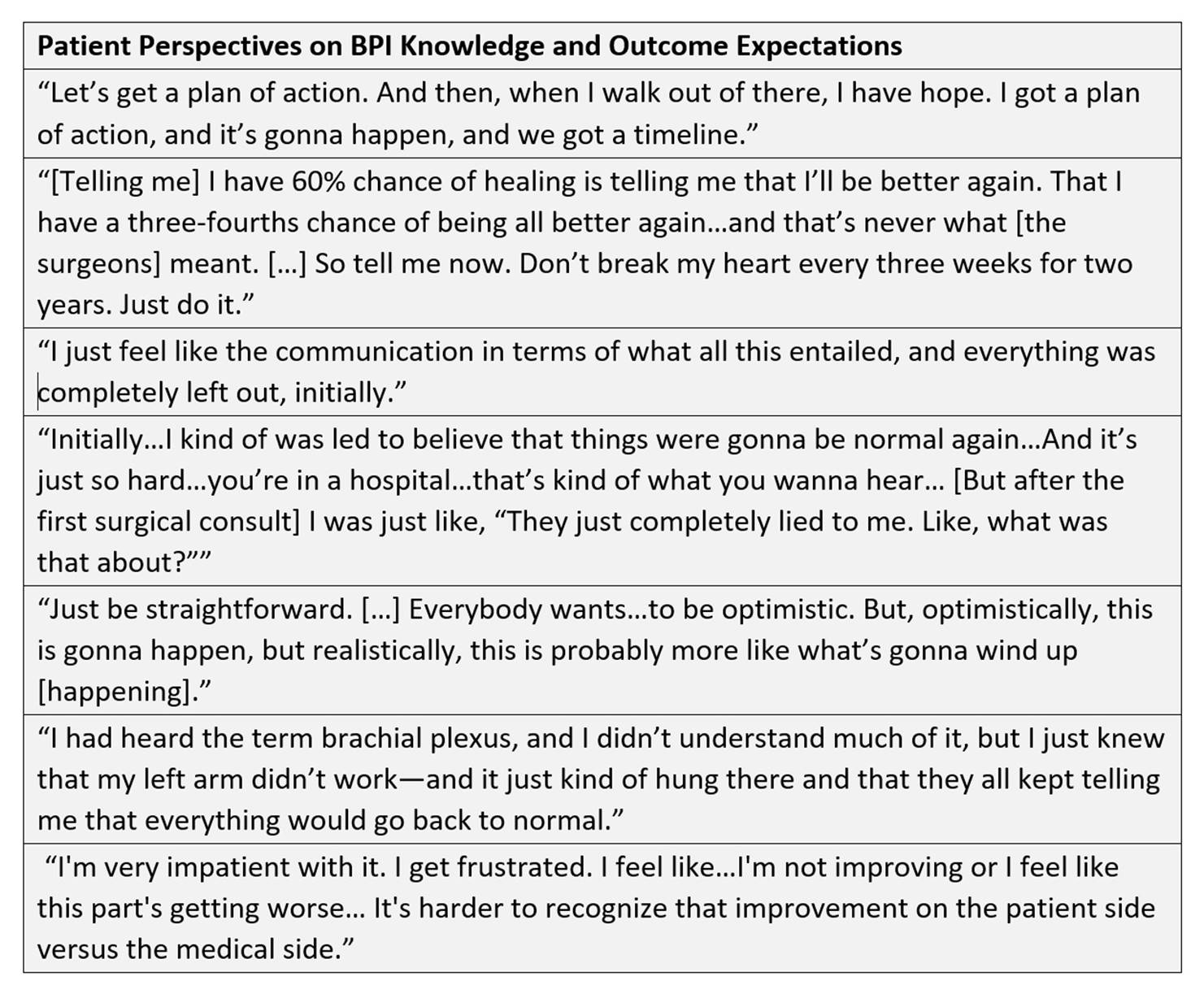
RESULTS: Patients described varying levels of understanding about their condition and prospects for recovery (Figure 1). Their knowledge was based on a variety of sources, with widely varying levels of accuracy. Many patients wanted a detailed explanation of what their ultimate injury outcome would be, or expressed a desire to have received “realistic” descriptions of their outcomes earlier in their treatment timeline. Some felt that having that information would allow them to make plans for their future, or come to terms with their “new normal”. Patients also described conversations with their surgeons regarding their expectations and estimated odds of recovery, which did not necessarily align with providers’ estimates of recovered function or degrees of recovery.
CONCLUSIONS: These results indicate substantial and highly variable knowledge gaps for BPI patients, and a communication disconnect that can lead to higher levels of patient frustration, decreased compliance with surgeon recommendations, and ultimately a detrimental effect on patient outcomes. Educating patients about their condition, the potential degrees of recovery they could see, and how their compliance with recommendations can specifically affect their recovery earlier in the patient’s treatment timeline has the potential to lead to more positive patient outcomes. Based on these findings, we are developing a patient-centered education tool specific to BPI that covers the knowledge gaps brought forward by patients.
FIGURE
Back to 2020 Abstracts