A Nationwide Cohort Study on Treatment and Survival in Patients with Malignant Peripheral Nerve Sheath Tumors.
Enrico Martin, MD1, J. Henk Coert, MD, PhD1, Uta E. Flucke, MD PhD1, Willem-Bart M. Slooff, MD1, Thijs van Dalen, MD, PhD1, Michiel A.J. van de Sande, MD, PhD2, Winan J. van Houdt, MD, PhD3, Dirk-Jan Grunhagen, MD, PhD4 and Cornelis Verhoef, MD, PhD4, (1)University Medical Center Utrecht, Utrecht, Netherlands, (2)Leiden University Medical Center, Leiden, Netherlands, (3)Netherlands Cancer Institute, Amsterdam, Netherlands, (4)Erasmus Medical Center, Rotterdam, Netherlands
Background: Despite curative intents of treatment in localized malignant peripheral nerve sheath tumors (MPNST), local recurrences and distant metastases are very common and survival remains poor. A better understanding of the clinical prognostic factors of this rare sarcoma is necessary to ameliorate clinical decision-making. This study set out to investigate overall survival, treatment modalities, and factors associated with survival in non-retroperitoneal and retroperitoneal MPNSTs using a Dutch nationwide cohort of patients.
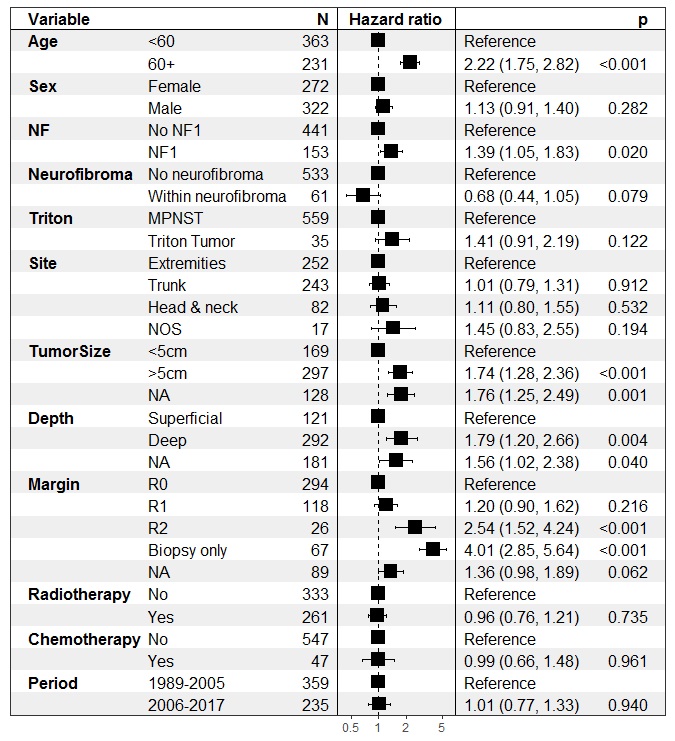
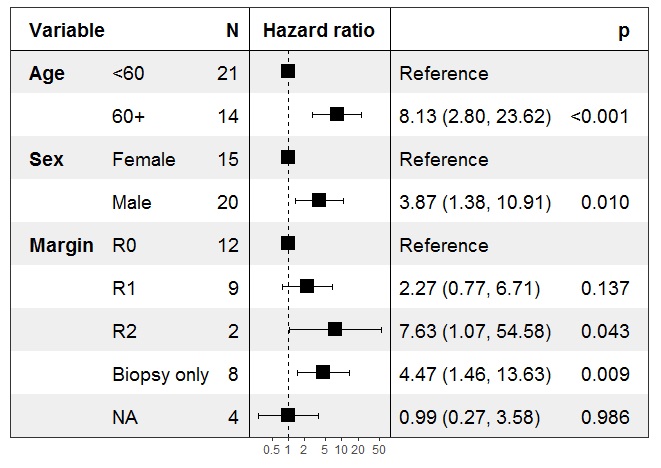
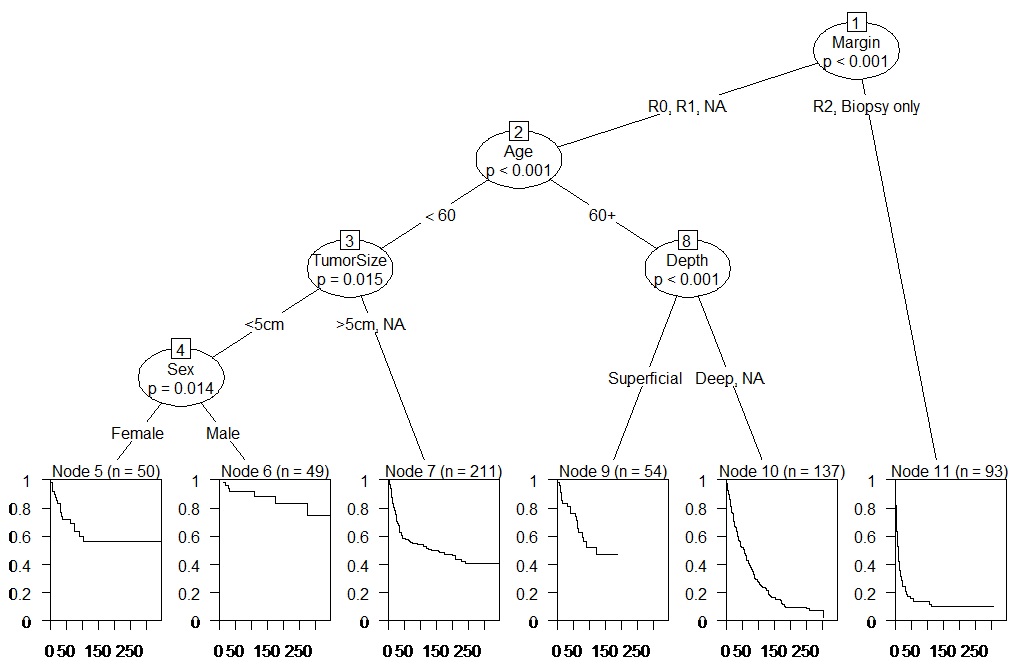
Methods: Data were obtained from the Netherlands Cancer Registry (NCR) and the Dutch Pathology Database (PALGA). All pathologically confirmed primary MPNSTs were collected. Patient and tumor characteristics, treatment modalities, and survival were extracted from the database and pathology reports. Pediatric cases (age ≤18 years) and patients with synchronous metastases were excluded from analyses. Separate Cox proportional hazard models were made for localized non-retroperitoneal (Figure 1) and retroperitoneal MPNSTs (Figure 2). A conditional inference tree was constructed for non-retroperitoneal localized MPNSTs (Figure 3).
Results: A total of 784 patients (26.8% neurofibromatosis type 1, NF1) had a final pathological diagnosis of MPNST. In 72 (9.2%) cases, MPNSTs arose within neurofibromas. Most MPNSTs arose in truncal sites (n=355, 45.2%) of which 43 (5.5%) were situated retroperitoneal. Most tumors were large (>5cm, 67.9%) and deep-seated (under the fascia, 75.2%). In 11.5%, patients presented with synchronous metastases. In localized MPNST surgical resection was performed in 88.1%. In surgically treated patients, radiotherapy was administered in 44.2% and less commonly in retroperitoneal tumors (29.6%, p<0.05). Chemotherapy was used in 6.7% of resected MPNSTs and more commonly in retroperitoneal tumors (18.5%, p<0.05). In non-retroperitoneal MPNST, older age (≥60), NF1 patients, large, and deep-seated tumors were independently associated with worse survival (p<0.05). MPNSTs arising within neurofibromas tended to do better (p>0.05). In retroperitoneal MPNST male sex and age ≥60 years old were independently associated with worse survival. R1 resections were not associated with worse survival in both non-retroperitoneal and retroperitoneal MPNST. Chemotherapy and radiotherapy use were not associated with survival in both models.
Conclusion: In localized MPNST, risk stratification for survival can be done using several patient- and tumor specific characteristics. Although MPNSTs can present diversely, achieving at least an R1 resection is the most important predictor for survival. Controlling for several factors, no significant difference in survival is seen between R0 and R1 resections. This is true for both retroperitoneal and non-retroperitoneal MPNSTs.
Figure 2
Figure 3
Back to 2020 Abstracts