Comparing Changes in Pain, Quality of Life, and Depression as Predictors of Post-Nerve Surgery Success
Kartemus Heary, BS1; Madeline Rose Thompson, BA1; Susan E. Mackinnon, MD2; Katherine Santosa, MD, MS3; Victoria Kaskutas, MHS, OTD4; Benjamin A. Philip, PhD1
1Washington University School of Medicine, St. Louis, MO, 2Department of Surgery, Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, St. Louis, MO, 3Section of Plastic and Reconstructive Surgery, University of Michigan, Ann Arbor, MI, 4Washington University in St. Louis, St. Louis, MO
Introduction Peripheral nerve injuries and disorders (PNID) can result in significant disability and loss of quality of life. Because chronic pain induces changes in the nervous system, nerve pain can linger even after the cause has been surgically addressed. Therefore, we predicted that pre- to post-operative changes in quality of life (qol) and depression might be more accurate early predictors of surgical success than changes in level of pain. The aim of this study was to compare changes in qol, depression, and pain in PNID patients as measured by self-reported visual analogue scales (VAS) from pre-operative visit (pre-op) to first post-operative visit (post-op) and final follow-up visit (final visit).
Materials & Methods:
We analyzed a pre-existing database of 464 PNID patients containing self-report VAS scores of level of pain, level of negative impact of injury on qol, and level of depression, each on a scale from 0 to 10, at three different time points: pre-op, post-op, and final visit. We used paired samples t-tests to determine if each of these three variables differed significantly from pre-op to post-op and from pre-op to final visit.
Results:
Average time from pre-op to surgery was 9 weeks (SD 15.8), from surgery to post-op was 4 weeks (SD 6.0), and from post-op to final visit was 23.5 (SD 24.5) weeks. Table 1 shows the mean scores for each measure at pre-op, post-op, and final visit, and the changes from pre-op to post-op and from post-op to final visit.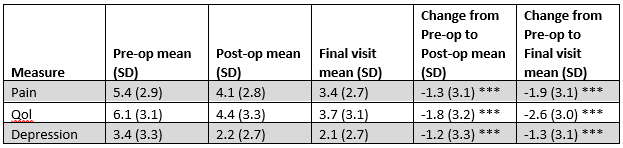
Table 1. Mean scores and changes from pre-op to post-op and final visit for pain, qol, and depression.
Conclusions:
Our results show that all three measures improved from pre-op to post-op and continued to improve from post-op to final visit. Depression and pain had improved similarly at post-op but pain had improved more than depression at final visit. All changes were significant (p < .001). Qol showed the greatest improvement, suggesting that measurement of changes in qol is a greater early predictor of surgical success than changes in pain or depression. A follow-up study expanding on these results and including measures of anger and frustration in a larger sample is underway.
Back to 2019 Abstracts
