Outcomes of Reconstructive Surgery in Traumatic Brachial Plexus Injury with Concomitant Vascular Injury
Alice E. Huang, BS1, Shelley S. Noland, MD2, Robert J. Spinner, MD3,4, Allen T. Bishop, MD3,4 and Alexander Y. Shin, MD3,4, (1)Mayo Clinic School of Medicine, Rochester, MN, (2)Mayo Clinic, Phoenix, AZ, (3)Mayo Clinic, Department of Orthopedic Surgery, Rochester, MN, (4)Mayo Clinic, Department of Neurological Surgery, Rochester, MN
Introduction: Adult traumatic brachial plexus injuries (AT-BPI) are devastating injuries that result in significant physical disability, psychological distress, and socioeconomic hardship. The outcomes of concomitant nerve and vascular injuries are rarely reported, generally not specific to AT-BPI, and often contradictory. The purpose of this study is to evaluate the functional and patient-reported outcomes of AT-BPI reconstruction in patients with associated vascular injury as well as address the significance and impact of location and type of vascular injury.
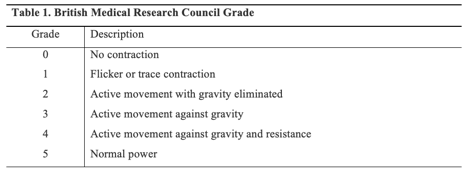
Methods: A retrospective review was performed of 325 patients with AT-BPI who underwent reconstructive surgery between 2001 and 2012. Patients with (vascular group) and without (control group) vascular injuries were identified by review of medical documentation. Patient presentation, characteristics of nerve and associated lesions, and surgical management were evaluated to identify prognostic variables. Postoperative muscle strength (measured according to the standardized British Medical Research Council grading system; Table 1), range of motion, and patient-reported disability scores were analyzed to determine long-term outcome.
Results: Sixty-eight patients had a concomitant vascular injury. There were no significant differences in age or sex between the control and vascular groups. Vascular patients were more likely to have pan-plexus lesions (p<0.0001), with significantly more associated upper extremity injuries (p<0.0001). The control group underwent more nerve transfers whereas vascular patients underwent more nerve grafting (p=0.003). Complete outcomes data were obtained in 139 patients, which included 111 control (43% of all controls) and 28 vascular patients (41%). There was no significant difference in patient-reported disability scores between the two groups. However, 73% of controls had grade 3 or greater postoperative elbow flexion while only 43% of vascular patients achieved these strengths (p=0.003; Table 2). Control patients demonstrated a greater increase in strength of shoulder abduction as well (p=0.004). Shoulder external rotation strength was grade 0 in the majority of patients, with no difference between the two groups.
Conclusions: Concomitant vascular injury leads to worse functional outcome following reconstructive surgery of traumatic brachial plexus injury.
Back to 2020 Abstracts