The Extent of Brachial Plexus Injury: A Forgotten Factor in Suprascapular to Spinal Accessory Nerve Outcomes
Kevin T Rezzadeh, BA1; David Daar, MD2; Jacques H. Hacquebord, MD1; Ajul Shah, MD3
1New York University School of Medicine, New York, NY, 2NYU Langone Medical Center, New York, NY, 3Section of Plastic Surgery, New York University, New York, NY
Introduction
Spinal accessory nerve (SAN) to suprascapular nerve (SSN) transfer is a common treatment in brachial plexus injury. A range of outcomes have been reported. The goal of this pooled analysis is to identify outcomes of SAN to SSN nerve transfer and factors predictive of improved outcomes. We hypothesize injury severity is predictive of worse outcome, and isolated use of SAN to SSN for shoulder reanimation deserves further scrutiny.
Methods
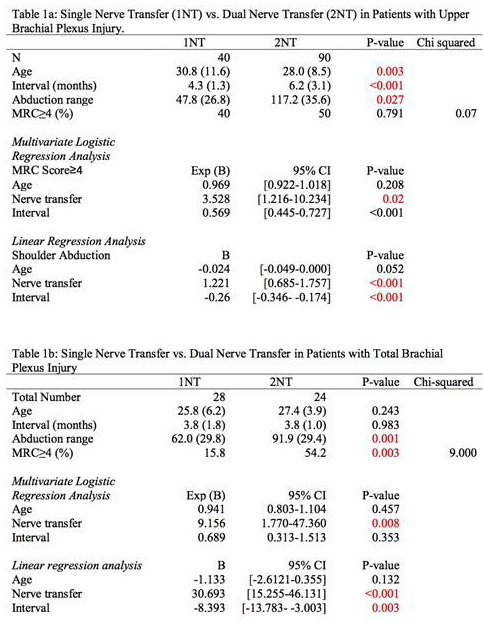
A combination of subject headings and keywords were searched across literature engines. Eligibility and exclusion criteria were applied. Patients were stratified based on upper plexus lesions (C5-6) or pan-plexus lesions (C5-T1). Then, they were categorized into two groups for analysis: single nerve transfer (SSN to SAN) or dual nerve transfer (SSN to SAN+axillary nerve [AXN] neurotization). Comparison was performed using chi-square and independent samples t-test. Linear regression, univariate and multivariable logistic regression analyses were used. Age, type of transfer, and interval from injury were explored as predictors of outcomes.
Results
14 studies were included for a total of 182 patients. Demographics demonstrate no significant differences other than age and interval between injury and surgery in patients with upper plexus injuries (p=0.003, <0.001). In patients with upper plexus injury, shoulder abduction was improved in patients receiving dual nerve transfer (p=0.027). In patients with total plexus injury, dual nerve transfer improved postoperative abduction range and attainment of shoulder MRC = 4 (p=0.001, p=0.003). Logistic and linear regression analyses demonstrate dual nerve transfer to be a statistically significant predictor of shoulder abduction MRC score = 4 in both upper and total brachial plexus injury. Shorter interval from injury to surgery was a predictor of better outcome in both injury types (p<0.001, p=0.003).
Conclusion
Patients with SAN to SSN attained the best results in the setting of dual nerve transfer and shorter interval to surgery. Importantly, increasing injury severity appears predictive for worse MRC outcome. This data demonstrates the need to question isolated usage of SAN to SSN for shoulder reanimation in severe injuries. Further studies will help inform the discussion on the indications for SAN to SSN nerve transfer for optimal postoperative outcomes.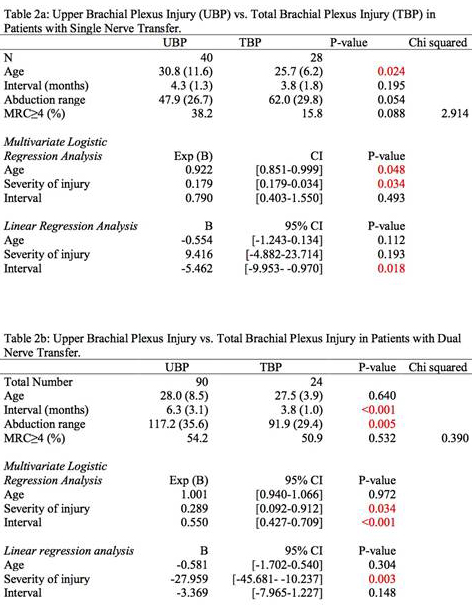
Back to 2019 ePosters
