Trends and Outcomes Between Direct Nerve Repair and Nerve Graft for the Treatment of Upper Extremity Peripheral Nerve Injury: Nationwide Analysis from 2002 to 2014
Neill Yun Li, MD; Justin E Kleiner, BS; Christopher J Got, MD
Alpert Medical School of Brown University, Providence, RI
Introduction:
Few studies have assessed how improvements in operative technique, materials, and grafts over the last decade have altered procedures used in upper extremity peripheral nerve injury. The purpose of this study was to compare trends and outcomes of nerve graft and nerve suture procedures following upper extremity peripheral nerve injury.
Methods:
The National Inpatient Sample (NIS) between 2002 and 2014 was queried for mixed and sensory upper extremity peripheral nerve injuries using ICD-9-CM diagnosis codes (Axillary: 955.0, Median: 955.1, Ulnar: 955.2, Radial: 955.3, Musculocutaneous: 955.4, Cutaneous: 955.5, Digital: 955.6). ICD-9-CM procedure codes isolated injuries undergoing nerve graft (045) or nerve suture (043). Age, sex, insurance, comorbidities, hospital setting, length of stay, total charges, and complications were extracted. Regression analyses were performed with p-values < 0.05 considered significant.
Results:
Between 2002 and 2014, there were 128,118 nerve injuries of which the proportion undergoing surgery remained consistent (p=0.231). During this time, suture repair decreased from 5,189 (94.7%) to 2,630 (85.4%)(p<0.001) as graft repair increased from 288 (5.26%) to 450 (14.6%)(p<0.001) (Figure 1). White patients, private insurance, injuries in more recent years, and care at teaching hospitals were more likely to have graft repair (p<0.05) whereas sensory nerves and female patients were less likely (p<0.001) (Table 1). Significant increase in total charges, length of stay, and complication rates in graft procedures were found compared to suture (p<0.01) (Table 2).
Conclusions:
Evaluation of upper extremity nerve injuries over 12 years found a decrease in suture and increase in graft repair. Patients undergoing graft placement were more likely to be white, male, with mixed nerve injury, private insurance, and present to a teaching hospital. Total charges, length of stay, and complication rates were significantly greater in graft than suture repairs. Differences in patient demographics and hospital setting may be a result of increased resources required to pursue graft procedures. Improvements in nerve repair should thus be offered in a cost-effective fashion to a wide demographic in different healthcare settings.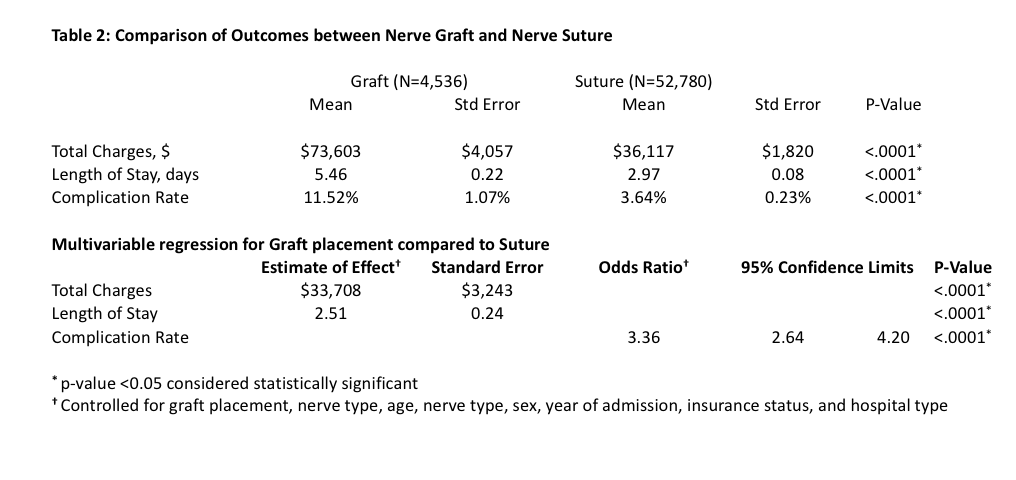
Back to 2019 ePosters
