The Implications Of Intradural Extension In Paraspinal Malignant Peripheral Nerve Sheath Tumors: Effects On Central Nervous System Metastases And Overall Survival
Hannah Gilder, MD; Ross Puffer, MD; Mohamad Bydon, MD; Robert J. Spinner, MD
Mayo Clinic, Rochester, MN
Object: In this study, we sought to compare tumors with intradural extension to those remaining in the epidural or paraspinal space with the hypothesis that intradural extension may be a mechanism for seeding of the cerebrospinal fluid (CSF) with malignant cells, thereby resulting in higher rates of CNS metastases and shorter overall survival
Methods: We searched the medical record for cases of MPNSTs identified from 1994 to 2017. The charts of the identified patients were then reviewed for tumor location in order to identify patients with paraspinal malignancy. All patients included in the study had tumor specimens reviewed by our surgical pathology department. Paraspinal tumors with intradural extension were identified in the lumbar, sacral, and spinal accessory nerves, and attempts were made to match this cohort by using patients who had paraspinal tumors of the cranial nerves and lumbar and sacral spinal regions without intradural extension. Further information was collected on all patients with and without intradural extension, including date of diagnosis by pathology specimen review, nerve or nerves of tumor origin, presence, location, and diagnostic date of any central nervous system (CNS) metastases, and either the date of death or date of last follow-up.
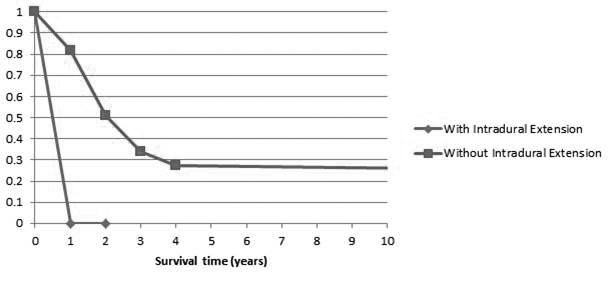
Results: We identified 6/179 (3.4%) patients who had intradural tumor extension, and they were compared to 12 patients with paraspinal tumors that did not have intradural extension (Figure 1). All tumors were diagnosed as high grade MPNST by surgical pathology. Four out of six (66.7%) patients with intradural extension had documented CNS metastases and The presence of CNS metastases was significantly higher in the intradural group compared to the paraspinal group (intradural – 66.7% vs. paraspinal – 0%, p <0.01). Time from diagnosis until death was 11.2 months in the intradural group, compared to approximately 72 months in the paraspinal, extradural cohort (Figure 2).
Conclusions: In patients with intradural extension of paraspinal MPNSTs, significantly higher rates of CNS metastases are seen with a reduced interval of time from diagnosis to metastatic lesion detection. Intradural tumor extension is also a poor prognostic factor for survival, with these patients showing a reduced mean time from diagnosis to death.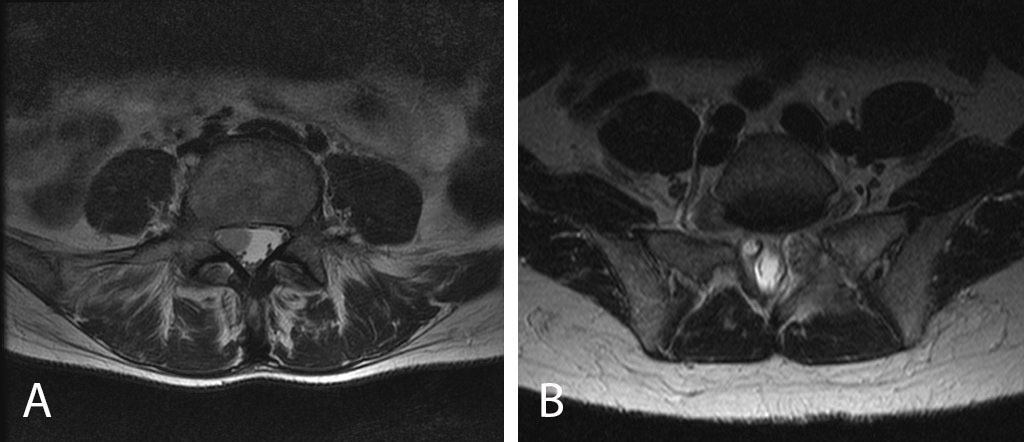
Back to 2019 ePosters
