New Persistent Opioid Use Among Patients Undergoing Common Peripheral Nerve Procedures
Katherine Santosa, MD, MS1; Hsou-Mei Hu, PhD, MBA, MHS2; Susan E. Mackinnon, MD3; Amy M Moore, MD3; Alison K. Snyder-Warwick, MD4; Jennifer F. Waljee, MD, MPH, MS5
1Section of Plastic and Reconstructive Surgery, University of Michigan, Ann Arbor, MI, 2University of Michigan, Ann Arbor, MI, 3Department of Surgery, Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, Saint Louis, MO, 4Washington University School of Medicine, St. Louis, MO, 5Section of Plastic Surgery, Department of Surgery, University of Michigan, Ann Arbor, MI
Introduction: Peripheral nerve procedures are commonly performed in the United States. Depending on the nerve, site, mechanism, and chronicity, patients often present with life-limiting pain. Managing pain after surgery may be especially challenging among this patient population given the known pathophysiological changes with regards to pain that occur with these conditions, such as brachial plexus injuries, cubital tunnel syndrome, and carpal tunnel syndrome among others. In this context, the goal of our study was to leverage a population-level dataset of insured individuals to determine the incidence of new persistent opioid use among opioid na´ve patients undergoing surgery for different types of peripheral nerve conditions.
Materials and Methods: We utilized the Truven Health MarketScan« databases to identify opioid na´ve (i.e. those who did not have an opioid prescription between 365 and 31 days prior to surgery) adult patients (18-64 years old) who underwent surgery for brachial plexus injuries, cubital tunnel syndrome, carpal tunnel syndrome, ulnar nerve compression at the wrist, and pathology of the peroneal and facial nerves between January 2012 to June 2016. Patients were followed for 6 months after their surgical date to define the incidence of new persistent opioid use, defined as an opioid prescription fill between 90 and 180 days after surgery. We also performed a logistic regression to identify risk factors for new persistent use.
Results: In total, 64.8% (239,328) of opioid naive patients who had peripheral nerve surgery filled an opioid prescription in the perioperative period (i.e. between 30 days before and 14 days after surgery). Across all procedure types, 8.3% of patients continued to fill opioid prescriptions between 90 and 180 days after surgery. Adjusted rates for new persistent use by surgery type are presented in Figure 1. Our logistic regression found that female sex, comprehensive insurance, higher Charlson comorbidity index, anxiety, mood disorder, drug and substance use disorders, presence of pain disorder, higher opioid dose of initial prescription, and use of adjunct neuropathic pain medications 30 days before to 14 days after were associated with an increased risk of new persistent opioid use.
Conclusions: About 8% of opioid na´ve patients continue to use opioids 90 days after peripheral nerve surgery. Identifying patients at highest risk and educating all-comers are necessary to curbing the prescription opioid drug crisis.
Figure 1.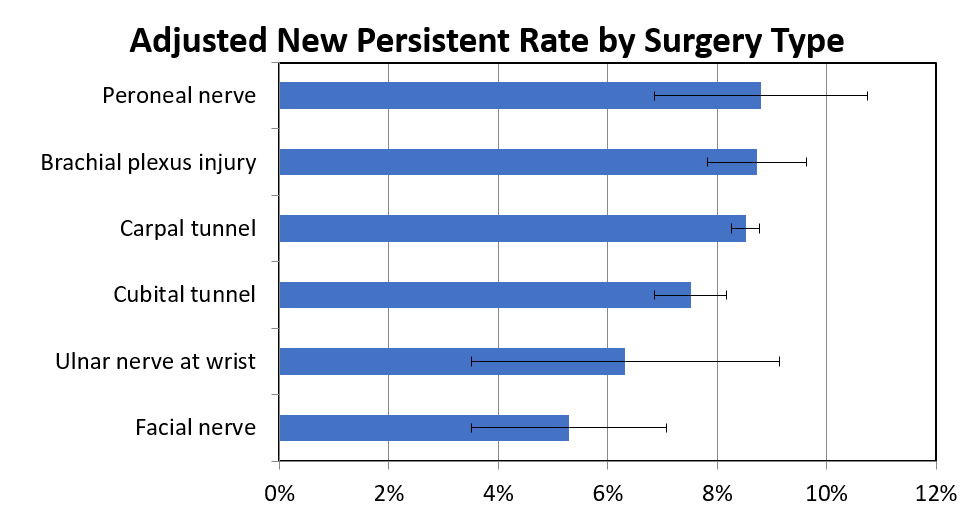
Back to 2019 ePosters
