Diagnostic Criteria for Symptomatic Neuroma
Denise Arnold, BA; Suzanne Caroline Wilkens, MD; Neal C Chen, MD; Ivica Ducic, MD, PhD; Kyle R Eberlin, MD;
Massachusetts General Hospital, Massachusetts General Hospital, Boston, MA
Introduction:
Following nerve injury, disorganized or incomplete nerve regeneration may result in a neuroma. The true incidence of symptomatic neuroma is unknown, and the diagnosis has traditionally been made based on patient history, symptoms, physical examination, and the anatomic location of pain, along with response to diagnostic injection. There are no formally accepted criteria for a diagnosis of neuroma.
Materials and Methods:
A literature search was performed to identify articles related to neuroma: PRISMA guidelines were followed and Pubmed, EMBASE and the Cochrane Library were searched for all relevant articles pertaining to neuroma (Figure 1). Articles were screened by title and abstract for relevance. If an article was considered potentially relevant, the full article was reviewed. After consideration, 50 articles were included in this systematic review.
Results:
No previous articles directly addressed diagnostic criteria for symptomatic neuroma. Factors related to neuroma diagnosis gleaned from prior studies include pain and cold intolerance (patient history), positive Tinel sign or diminished two point discrimination (physical examination findings), response to diagnostic nerve block, and presence of neuroma on diagnostic imaging (ultrasound or MRI). Based on literature review, the importance and number of references, as well as clinical experience, we propose criteria for diagnosis of symptomatic neuroma (Figure 2). To receive a diagnosis of symptomatic neuroma, patients must have (1) pain with at least 3 qualifying “neuropathic” characteristics, (2) symptoms in a defined neural anatomic distribution, and (3) a history of a nerve injury or suspected nerve injury. In addition, patients must have at least two of the following four findings: (1) positive Tinel sign on examination at/along suspected nerve injury site, (2) tenderness/pain on examination at/along suspected nerve injury site, (3) positive response to a diagnostic local anesthetic injection, and (4) US or MRI confirmation of neuroma.
Conclusions:
The diagnosis of neuroma is based on a careful history and physical examination, and should rely on the proposed criteria for confirmation. These criteria will be helpful in more precisely defining the diagnosis for clinical and research purposes.
Figure 1: PRISMA 2009 Flow Diagram for inclusion of articles into systematic review
Figure 2: Diagnostic Criteria for Neuroma 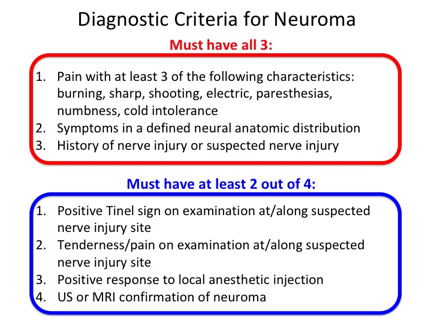
Back to 2019 ePosters
