Sub-Clinical Peroneal Neuropathy is Common and Associated with Falling in Ambulatory, Community Dwelling Adults
Louis H Poppler, MD, MSCI1; Jenny Yu, MD1; Susan E. Mackinnon, MD2; (1)Washington University in St. Louis, St. Louis, MO, (2)Department of Surgery, Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, Saint Louis, MO
Introduction: Peroneal neuropathy with an overt foot drop is a known risk factor for falling. Sub-clinical peroneal neuropathy (SCPN) due to compression at the fibular head is more subtle and does not have an obvious foot drop. SCPN was previously found in 31% hospitalized patients and was associated with having fallen. The prevalence of SCPN among ambulatory outpatients is unknown. Identification and treatment of SCPN may reduce fall incidence. This study’s purpose is to determine the prevalence of SCPN in ambulatory outpatients and establish if it is associated with falling.
Methods: A prospective, cross-sectional study of 398 ambulatory outpatients presenting to the plastic and orthopaedic surgical clinics at a large academic tertiary care hospital was performed. Patients referred for peroneal neuropathy were excluded. Patients were examined for findings that suggest peroneal neuropathy, fall risk, and a history of falling. Multivariate logistic regression was used to correlate SCPN with fall risk (Activity and Balance Confidence (ABC) Scale) and a history of multiple falls in the past year.
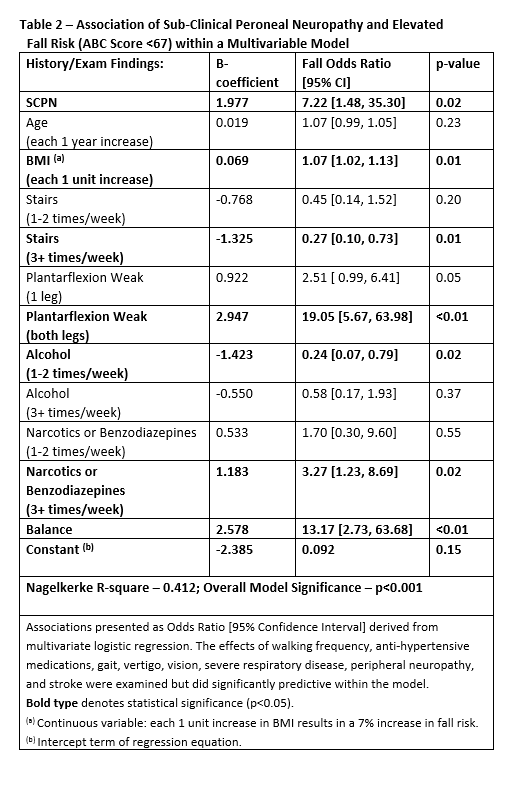
Results: The mean age of enrolled patients was 54 ± 15 years and 248 (62%) were female. The population was active with 344 patients (86%) walking more than 30 minutes and 361 (91%) taking a flight of stairs at least one or two times weekly. Thirteen patients (3.3%) were found to have SCPN. Two patients (0.5%) had bilateral SCPN. After controlling for various factors known to increase fall risk, patients with SCPN were 3.74 times [95% confidence interval: 1.06 - 13.14] (p=0.04) more likely to report having fallen multiple times in the past year than patients without SCPN (Table 1). Similarly, patients with SCPN were 7.22 times [95% confidence interval: 1.48 - 35.30] (p=0.02) more likely to have an elevated fall risk on the ABC fall risk scale (Table 2). As the number of lower extremities affected increased, the strength of association increased suggesting a cause-effect relationship between SCPN and falling.
Conclusions: SCPN is common, affecting 3.3% of ambulatory outpatients, and associated with falling in this active population. Future studies are needed to see if therapy or surgery to treat SCPN reduce fall incidence in this population.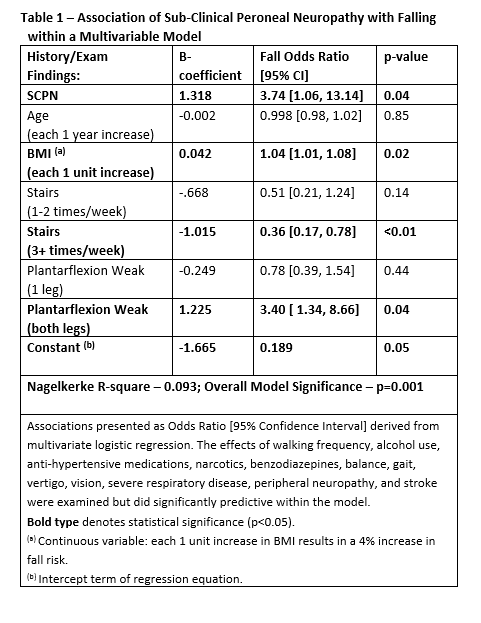
Back to 2018 Program
