Photochemical Tissue Bonding Optimizes Outcomes of Large Gap Peripheral Nerve Defects Repaired with Acellular Nerve Grafts in a Porcine Model
Rachel L Goldstein, D.O.1,2; Mark A Randolph, MAS3; Gem Runyan, B.S., M.S.1; Jeena M Easow, MD3; William S David, M.D., PhD1; Robert W Redmond, PhD4; Jonathan M Winograd, MD3; (1)Massachusetts General Hospital, Boston, MA, (2)The Wellman Center for Photomedicine, Boston, MA, (3)Plastic and Reconstructive Surgery, Massachusetts General Hospital, Boston, MA, (4)Wellman Center for Photomedicine, Massachusetts General Hospital, Boston, MA
Background: Standard reconstruction of large gap peripheral nerve defects requires a nerve autograft harvested from a donor limb. This is not always available after massive traumas, as in battlefield situations. An alternative, acellular nerve graft, is associated with suboptimal outcomes. Multiple nerve repair studies demonstrate a benefit using photochemical tissue bonding (PTB) to create a seal of cross-linked collagen across coaptation sites. In our recent small animal studies, PTB improved outcomes when used with acellular grafts to repair large gap nerve defects, compared to standard sutured autograft repair. We now investigate this treatment in a large animal model to achieve clinical relevance.
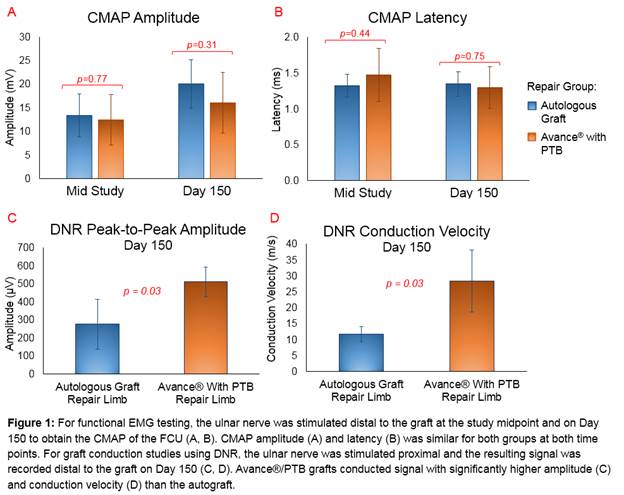
Materials & Methods: Six miniature swine underwent bilateral ulnar nerve resection. In each pig, 5-cm nerve defects were repaired with sutured saphenous nerve autograft in the control limb, and acellular human nerve graft, Avance«, with PTB in the experimental limb. For PTB, human amniotic membrane (HAM), coated with photosensitizing dye, Rose Bengal, was wrapped around neurorrhaphy sites, then exposed to green light inducing collagen cross-linking. Tacrolimus prevented reaction to xenografts. Functional electromyography (EMG) at the study midpoint and Day 150, measured the compound muscle action potential (CMAP) of the flexor carpi ulnaris (FCU). Graft conduction was measured on Day 150 with direct nerve recording (DNR). On Day 150, animals were euthanized and grafted ulnar nerves and FCU muscles collected for histology.
Results: Five pigs survived the five-month study. There were no gross differences in grafts at harvest. At both the study midpoint and on Day 150, CMAPs in limbs repaired with autologous graft and Avance«/PTB were not statistically different in amplitude (respectively, p=0.77 and 0.31) and latency (respectively, p=0.44 and 0.75). With DNR, compared to autologous grafts, Avance«/PTB grafts conducted signals with significantly higher amplitude (respectively, 275▒138 vs 510▒82 ÁV, p=0.03) and conduction velocity (respectively, 11.7▒2.4 vs 28.4▒9.7 m/s, p=0.04) on Day 150 [FIGURE 1]. On histology, axon regeneration was present distal to both grafts, and FCU muscle fibers appeared similar in both limbs.
Conclusions: When PTB is used with acellular grafts to repair large gap nerve defects, graft conduction is improved and functional electrophysiologic outcomes are comparable to the standard repair. Functionality may be optimized for patients with large gap nerve injuries and no available donor limb by photochemically sealing coaptation sites.
Back to 2018 Program
