Surgical Management of Post-Traumatic Supraorbital and Supratrochlear Neuromas
Robin S Yang, M.D.; Johns Hopkins, Baltimore, MD; Chopra Karan, MD; Johns Hopkins, baltimore, MD; Eric Howard Williams, M.D.; Johns Hopkins School of Medicine Division of Plastic Surgery, Dellon Institute for Peripheral Nerve Surgery, Towson, MD; A. Lee Dellon, M.D., Ph.D.; Plastic Surgery, Johns Hopkins, Baltimore, MD
Introduction
Trauma to the supraorbital ridge is an under-appreciated and underdiagnosed source of pain. Blunt and penetrating trauma, aesthetic surgery, and craniofacial/neurosurgical procedures are potentional sources of injury to the supraorbital (SO) and or supratrochlear (ST) nerves. Pain related to injuries of these nerves can cause intractable headaches, and dysesthesias in the frontal-orbital facial region. Management of these nerve injuries is relatively under-reported. We present our experience with surgical management of SO and ST neuromas with nerve resection and implantation of the proximal nerve deep within the orbital cavity.
Methods and Materials
A retrospective, chart-review, study was performed. Patients included into the study were those who had direct trauma/injury to the supra-orbital region. All patients included in the study had failed at least one year of medical management and pain control prior to surgery. All patients had symptom relief with a pre-surgical nerve block of the SO and ST nerves. All patients included received similar surgical intervention, which was to divide the SO and ST nerves within the orbit through an upper blepharoplasty incision.
15 patients were identified who met the inclusion criteria. The patients age raged from 18-75 with an average of 50.5 years. Mechanism of Injury: Trauma = 12 Craniofacial/Neurosurgery = 2 Cosmetic procedure = 1. Unilateral Resection = 7 Bilateral Resection = 5
Results
Mean follow up: 16 month. Pre-operative VAS: 9.4/10 Post-Operative VAS: 2.6/10 (p <.001). All patients had a good or excellent outcome. No pain with extraocular eye movement. No wound complications.
Conclusion
This is the first report of successful treatment of neuromas of the SO and ST nerves by resection of neuroma and placement of the proximal ends within the orbital cavity. There was satisfactory relief of neuropathic pain with this surgical technique without any pain within the implantation site with ocular movement.
Figures:
A. B.
A.
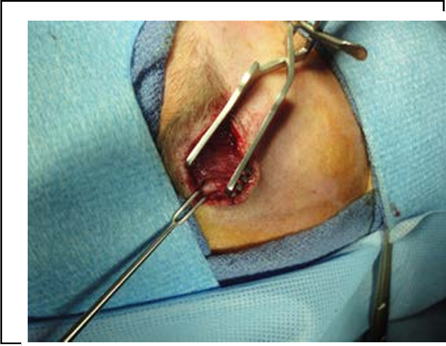

SO Nerve prior to resection B. SO Nerve resection prior to implantation
Back to 2018 Program
