Treatment and survival in malignant peripheral nerve sheath tumors: a SEER database analysis per tumor site
Enrico Martin, BS1,2; Ivo S. Muskens, BS1,2; Timothy R. Smith, MD, PhD, MPH1; Marike L.D. Broekman, MD, PhD, JD1,2; (1)Brigham & Women's Hospital, Harvard Medical School, Boston, MA, (2)University Medical Center Utrecht, Utrecht, Netherlands
Abstract
Background: Currently, literature is lacking data on differences across tumor sites in survival and treatment in malignant peripheral nerve sheath tumors (MPNSTs). The Surveillance, Epidemiology, and End Results (SEER) database provides a means of assessing possible predictive factors of survival and treatment strategies.
Methods: MPNST cases were obtained from the SEER program from 1973-2013. Tumor sites were recoded into: intracranial, spinal, head and neck (H&N), limbs, core, and unknown. Patient and tumor characteristics, treatment modalities, and survival were extracted. Overall survival was assessed using univariate and multivariate cox-regression hazard models and Kaplan-Meier survival curves were constructed per tumor site for overall survival (OS) and disease specific survival (DSS). Only primary tumors were used for survival analyses.
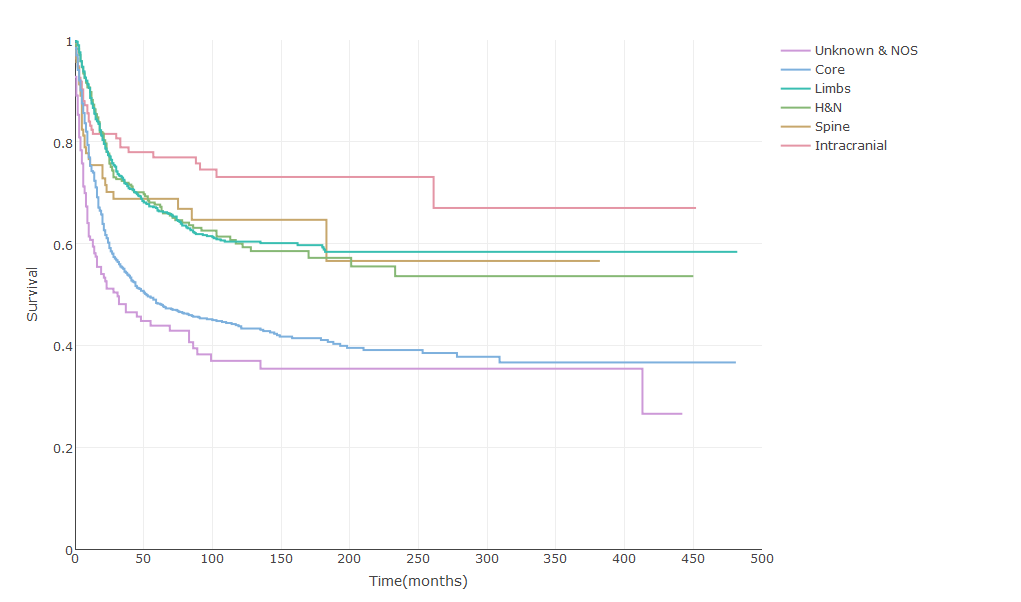
Results: 3267 MPNST patients were registered in SEER; 167 intracranial (5.1%), 119 spinal (3.6%), 449 H&N (13.7%), 1022 limb (31.3%), 1307 core (40.0%), and 203 unknown (6.2%). The largest tumors were found in core (size: 80.0mm, IQR: 60.0-115.0mm) and limb sites (size: 70.0mm, IQR: 40.0-100.0mm), and the smallest were intracranial (size: 37.4mm, IQR: 17.3-43.5). Intracranial tumors were resected least frequently (58.1%), whereas spinal tumors were most often resected (83.0%). Gross total resection was most commonly achieved in spinal tumors (42.6%) and least frequently in core tumors (24.9%). Radiation was administered in 35.5% intracranial and 41.8% limb MPNSTs. Independent factors negatively influencing survival were: older age, male sex, black race, no surgery, not gross total resection, large tumor size, high tumor grade, H&N site, and core site (all p<0.05). Intracranial and pediatric tumors showed superior survival (both p<0.05). Patients with intracranial tumors showed superior OS (Figure 1) and DSS curves (Figure 2), whereas core tumors had the worst OS and DSS (p<0.001).
Conclusion: Treatment modalities, extent of resection, and tumor size vary across primary tumor sites. Best survival was seen in intracranial MPNSTs, whereas core and H&N tumors had a worse prognosis.
Figure 1. Overall Survival in MPNST per Site
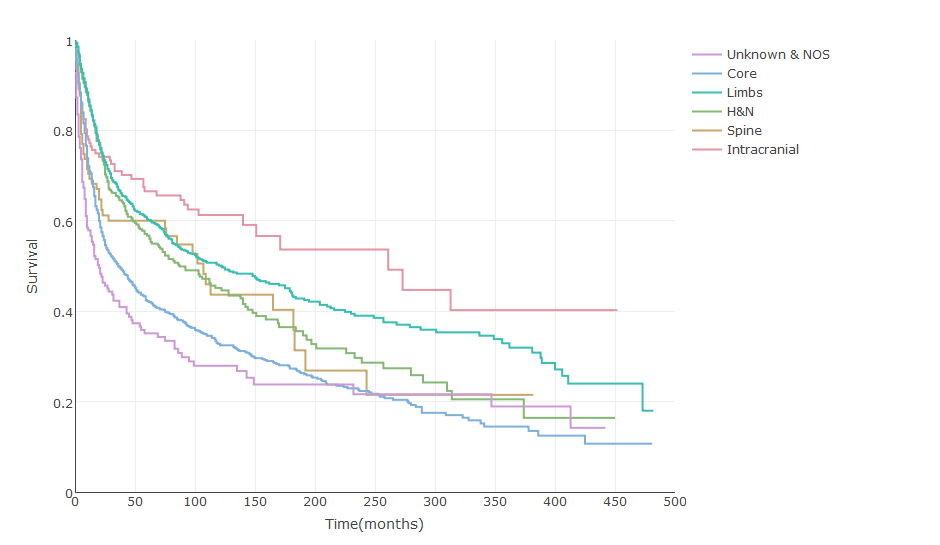
Figure 2. Disease-Specific Survival in MPNST per Site
Back to 2018 Program
