Motor Functional Recovery after Median Nerve Reconstructions using Processed Nerve Allografts
Bauback Safa, MD1; Timothy R Niacaris, MD, PhD2; Steven Maschke, MD3; John V Ingari, MD4; Jaimie T Shores, MD4; Harry Hoyen, MD5; Mickey Cho, MD6; Leon J Nesti, MD, PhD7; Gregory Buncke, MD1; (1)The Buncke Clinic, San Francisco, CA, (2)UNT Health Science Center, Fort Worth, TX, (3)Cleveland Clinic, Cleveland, OH, (4)Johns Hopkins Medicine, Baltimore, MD, (5)MetroHealth System, Cleveland, OH, (6)Orthopedics, San Antonio Military Medical Center, San Antonio, TX, (7)Walter Reed National Military Medical Center, Bethesda, MD
Introduction
Processed Nerve allografts (PNA) have seen increased utility for reconstruction of peripheral nerve injury. The RANGER® registry is an ongoing study that collects data on the utilization and outcomes of PNA (Avance® Nerve Graft, AxoGen) in peripheral nerve repair. Favorable outcomes have been demonstrated in an interim analysis of the expanding dataset. While a large proportion includes sensory nerve injuries due to the higher rates of incidence, the database also contains a significant number of major peripheral nerves repairs allowing for the evaluation of specific injury types. This current analysis was conducted to evaluate the motor functional outcomes after median nerve injuries repaired with PNA.
Materials & Methods
The RANGER database was queried for median nerve transections repaired with PNA that met following criteria: nerve transections distal to the elbow, repairs within six months (180 days) after injury; a minimum of six months of follow-up assessments; documented relevant motor function assessments sufficient for outcome evaluation using the Medical Research Council (MRC) scale.
For median nerve repairs at forearm level, motor function assessment included flexion of the thumb, index and middle fingers as well as the ability to form a composite fist; for repairs at wrist and recurrent motor branch level, assessment included palmar abduction of the thumb, flexion of the index and middle fingers at metacarpophalangeal joints. Meaningful recovery was defined as MRC scale ?M3.
Results
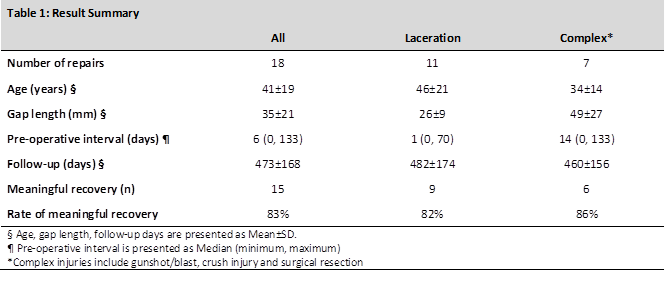
There were 18 median nerve repairs that met the inclusion criteria. Eight occurred at the forearm, eight at the wrist, and two at the recurrent motor branch level. Subjects in this cohort had a mean age of 41±19 years. The average gap length of nerve injuries was 35±21 mm. Subjects were followed for an average of 473±168 days. Fifteen (83%) of the repairs reported a MRC scale of ?M3. While complex injuries had longer gaps, no significant difference in meaningful recovery was seen between the groups. See Table 1. These results compare favorably to the rate of meaningful recovery with nerve autograft reported in the literature.
Conclusions
Repair of median nerves using processed nerve allografts after injury resulted in promising motor functional recovery. Processed nerve allograft represents a viable option for reconstruction of mixed nerves injuries. Outcomes compared favorably to that of nerve autograft reported in literature.
Back to 2018 Program
