The Prevalence and Practice Patterns of Human Acellular Nerve Allograft Use in Digital Nerve Gaps: a Survey of Hand Surgeons
Heather Lucas, PA-C1; Solomon Azouz, MD2; Raman C. Mahabir, MD, MSc1; Shelley S. Noland, MD3; (1)Plastic Surgery, Mayo Clinic, Phoenix, AZ, (2)Mayo Clinic, Phoenix, AZ, (3)Department of Orthopaedics and Sports Medicine, Mayo Clinic, Phoenix, AZ
Introduction:
The use of human acellular nerve allograft (HANA) for digital nerve gaps has become increasingly popular. Current state of adoption and coding practices by hand surgeons has not yet been reported.
Materials & Methods:
A twenty-six-question electronic survey of hand surgeons was performed to evaluate current practice patterns and coding of HANA.
Results:
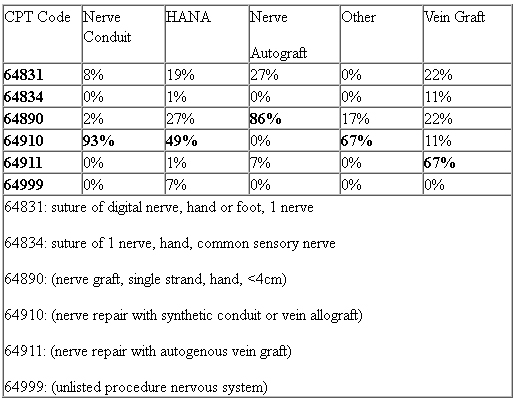
Of the 461 responses, the majority were trained in orthopedic surgery (76%) or plastic surgery (19%). There was a wide range of years in practice with 38% practicing less than 10 years, 24% practicing 11-20 years, and 36% practicing for more than 20 years. For those who completed a fellowship, 98% completed a hand surgery fellowship, 11% completed a peripheral nerve fellowship, and 7% completed a different fellowship. Most respondents reported using HANA (70%). Of those who do use HANA, nearly all use it less than 10 times/month (98%). There was no significant difference in the use of HANA across different specialties (p=0.41) but there was a significant difference in the use of HANA depending on the type of practice (p=0.0047), number of years in practice (p=0.0001), and the volume of nerve cases per month (p=0.0367). For all respondents, when presented with the clinical scenario of a 2 cm digital nerve gap, 39% would use HANA, 35% would use nerve conduit, and 21% would use nerve autograft (Figure 1). The most common CPT code selected was 64910 (nerve repair with synthetic conduit or vein allograft, 49%) followed by 64890 (nerve graft, single strand, hand, <4cm, 27%) (Figure 2).
Conclusions:
The majority of hand surgeons (70%) report using HANA in their practice. For the repair of 2 cm digital nerve gaps, HANA use has surpassed both nerve conduits and nerve autograft. Coding for the use of HANA was inconsistent and there may be a role for further clarification of proper coding.
Figure 1.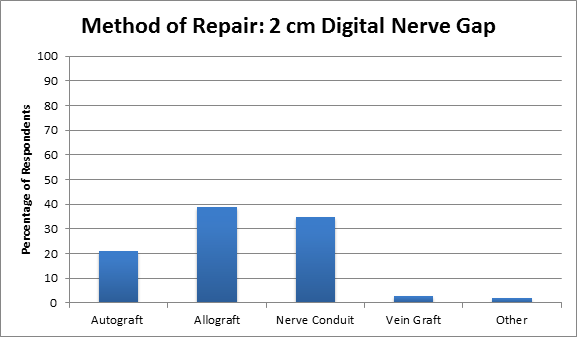
Figure 2.
Back to 2018 Program
