Cross-Cross Sensory Nerve Grafts to Enhance Sensory Recovery in Complex Ulnar Neuropathy
John M Felder, MD1; Hollie Power, MD1; Elspeth Hill, MD1; Jessica Hasak, RN1; Susan E. Mackinnon, MD2; (1)Washington University, St Louis, MO, (2)Department of Surgery, Division of Plastic and Reconstructive Surgery, Washington University School of Medicine, Saint Louis, MO
Introduction:
Debilitating sensory loss is a prominent feature of severe ulnar neuropathy with few surgical options proposed to improve recovery. Here we report our experience with side-to-side sensory nerve grafting from the median to ulnar nerve (‘cross-cross grafts’) to enhance sensory recovery.
Methods:
Cross-cross nerve grafting involves tension-free grafting from the sensory component of the median nerve to the sensory component of the ulnar nerve, in the palm, in a side-to-side fashion, employing short segment allo or autograft.
A retrospective chart review was performed to identifying patients with severe ulnar neuropathy who underwent cross-cross nerve grafting to enhance sensory. Patients were included if they had objective loss of protective sensation in the ulnar distribution with 2-point discrimination >8mm, Semmes-Weinstein monofilament testing (SWMT) >4.56 or no sensory response on nerve conduction testing. These patients underwent cross-cross nerve grafting from the sensory component of the median nerve to the sensory component of the ulnar nerve in the palm. Analysis included assessment of patient aetiology, procedures, nerve conduction studies, objective sensory testing and DASH disability score.
Results:
48 patients underwent cross-cross nerve grafting at our institution between 2014-2017. Of these, 20 patients had severe cubital tunnel syndrome, 7 had brachial plexus injury, 4 had ulnar nerve lacerations and 2 cervical radiculopathies. Of the patients with cubital tunnel syndrome, 60% were revisionary cases. 33 patients had anterior transposition of the ulnar nerve at the elbow and 32 also had a supercharged end-to-side AIN to ulnar nerve transfer. 24 patients had documented loss of ulnar protective sensation or 2 point discrimination >8 mm pre-operatively, and had adequate follow up for inclusion. 21 out of 24 patients (87%) had return of protective sensation within 1 year as assessed by SWMT and/or 2-point discrimination. DASH disability scores improved significantly. Technique and case examples are presented.
Conclusions:
Cross-cross nerve grafting may be a useful adjunct to enhance sensory recovery in patients with complex ulnar neuropathy. Further study to quantify the difference in sensory recovery with traditional operative techniques and cross-cross nerve grafting is required.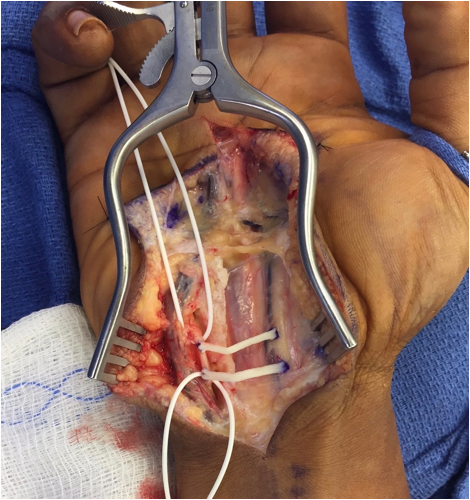
Back to 2018 Program
