Socioeconomic Disparities in the Receipt of Brachial Plexus Surgery: A National Analysis
Alexandra Bucknor, MBBS, MRCS, MSc1; Sabine A. Egeler, MD1; Anmol Chattha, BA2; Samuel J. Lin, MD, MBA, FACS1; Anne Huang, MD1
1Beth Israel Deaconess Medical Center / Harvard Medical School, Boston, MA; 2Albany Medical College, Boston, MA
Introduction
Previous studies have highlighted the disparities present in the provision of upper limb services within the United States. This study aims to characterize socioeconomic disparities and regional variation in an adult population with brachial plexus injuries.
Methods
Analysis of the Healthcare Cost and Utilization Project National Inpatient Sample Database (NIS) for the years 2009-2014 was undertaken. Data for adults with a primary diagnosis of brachial plexus injury with or without nerve repair during an emergency admission were retrieved using International Classification of Diseases Clinical Modification Ninth Revision codes 3530 and 9534. Patient and hospital level characteristics in addition to concomitant injuries were analyzed and the impact on receipt of brachial plexus surgery was assessed using a multivariable binary logistic regression model. The impact of surgery on discharge status (home or supported) was also assessed.
Results
Over the six-year study period, data for 5,355 cases were retrieved; of these, 494(9.2%) underwent brachial plexus surgery during their admission. Overall, a majority were white (64.8%) males (50.7%) most commonly aged 34-55 (40.1%), treated at large bed size (75.0%), non-teaching (72.0%) hospitals in the South (33.5%); 5.2% had a concomitant major orthopaedic injury. After adjustment, factors decreasing the odds of surgery were older age (35-54 years: OR 0.737, CI 0.578-0.939; 55+ years: OR 0.532, 0.376-0.754), Hispanic (OR 0.352, CI 0.205-0.604) or other non-African American racial minority (OR 0.405, CI 0.216-0.759), medium (OR 0.145, CI 0.088-0.239) or large bed size hospital (OR 0.553, CI 0.396-0.773), teaching hospital (OR 0.450, CI 0.341-0.592), and highest three income quartiles compared with the lowest (p<0.001). Patients had increased odds of having surgery if they had private insurance compared with Medicare/Medicaid (OR 1.411, CI 1.084-1.838). Results are summarized in table 1. On multivariable analysis, those undergoing brachial plexus surgery were significantly less likely to require supported discharge (OR 0.515, CI 0.350-0.759).
Conclusions
Results suggest that those undergoing brachial plexus nerve repair during the acute admission are more likely to be discharged home, rather than to supported care. Despite this, there are evident socioeconomic disparities in the receipt of brachial plexus surgery, particularly affecting certain racial minorities and those with government-based insurance. This may suggest a need for a centralized referral system to help improve access to more vulnerable populations.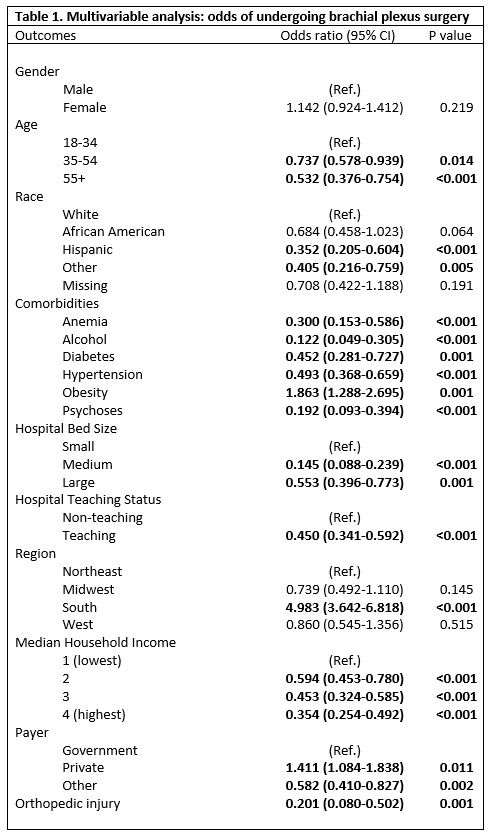
Back to 2018 ePosters
