Back to 2017 Annual Meeting Program
Functional Motor Recovery Outcomes after Repair of Traumatic Nerve Injuries Using Processed Nerve Allograft
Jaimie T Shores, MD1; John V Ingari, MD1; Jozef Zoldos, MD2; Renata V. Weber, MD3; Mickey Cho, MD4; Wesley Thayer, MD, PhD5; Bauback Safa, MD6
1Johns Hopkins Medicine, Baltimore, MD; 2Arizona Center for Hand Surgery, Phoenix, AZ, 3Institute for Nerve, Hand, and Reconstructive Surgery, Rutherford, NJ, 4Orthopedics, San Antonio Military Medical Center, San Antonio, TX, 5Department of Plastic Surgery, Vanderbilt University, Nashville, TN, 6The Buncke Clinic, San Francisco, CA
Introduction: While severe trauma to the upper extremities often results in the transection of major peripheral nerves, conducting controlled prospective clinical studies in this population remains a challenge. The RANGER® Registry is an ongoing observational study collecting data on the use and outcomes of processed nerve allograft (Avance® Nerve Graft, AxoGen, Inc.). The database includes a broad spectrum of nerve types, injury locations and mechanisms. In the current study, we reviewed the outcomes of using PNA to reconstruct mixed or motor nerve defect in the upper extremity, head and neck area. Meaningful recovery of motor function after these repairs is reported.
Methods: The RANGER database was queried for mixed or motor nerve injuries in the upper extremity, head and neck area that were repaired with PNA and reported sufficient follow-up assessments. Motor function assessments included range of motion and/or muscle strength tests. Reported quantitative outcome data were incorporated into the Medical Research Council Classification (MRCC) scale for motor function. Meaningful recovery was defined as ≥ M3 on the MRCC scale. Outcomes were compared to historical literature on nerve autograft and conduit.
Results: There were 31 nerve repairs in the cohort that reported sufficient outcome data for quantitative assessment of motor function after repair. The nerves repaired included: axillary, musculocutaneous, median, radial and ulnar nerve in the upper extremity, and spinal accessory, buccal, zygomatic, marginal mandibular nerve in the head/neck region. Mean age of the cohort was 40 ± 19(18 –77) years. Mean gap length was 28 ± 13(10–65) mm with a mean follow-up duration longer than a year (376 ±197 days). Meaningful recovery was observed in 81% of repairs. Analysis by mechanism of injury observed meaningful recovery in 88% of laceration and 73% of complex injuries. Demographics of these repairs are summarized in Table 1. No adverse events were reported.
Conclusion: Reconstruction of mixed and motor nerve defects using PNA resulted in good motor functional recovery in gaps between 10 and 65mm in length. Current data from the RANGER registry showed that 81% of these repairs achieved meaningful recovery of motor function after surgery. Outcomes compare favorably to historical controls from available literature for nerve autograft and exceed that of nerve conduit. The RANGER® registry is currently ongoing and future reports will provide additional clinical evidence on the expanding role of PNA in mixed and motor nerve repairs.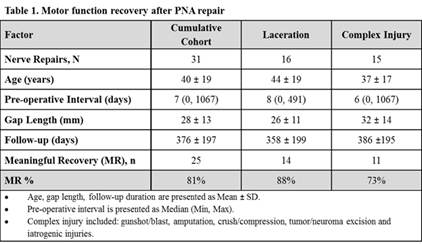
Back to 2017 Annual Meeting Program
