Back to 2017 Annual Meeting Program
Brain Metastasis from Malignant Peripheral Nerve Sheath Tumors
Ross Puffer, MD; Christopher Graffeo, MD; Grant Mallory, MD; Mark E. Jentoft, MD; Robert J. Spinner, MD
Mayo Clinic, Rochester, MN
Introduction: Metastatic disease is a well-known sequela of malignant peripheral nerve sheath tumors (MPNSTs). Metastatic spread to the brain is unusual.
Case Report: A 56-year-old man was found to have a high grade MPNST of the sciatic nerve. Despite en-bloc excision of the sciatic nerve and local radiation post-operatively, he developed pathologically confirmed systemic metastases: 25 months after the diagnosis he was found to have lung nodules and received chemotherapy; and thirty-two months after initial diagnosis, he presented with left leg weakness and sensory changes and was found to have a lesion of the frontal lobe, received palliative radiation following which he developed systemic metastases and died 35 months after initial presentation. Review of a clinical cohort: We retrospectively reviewed the charts of 179 patients treated at our institution with MPNSTs since 1994. This was the only case of a pathology proven brain metastasis, resulting in an incidence of 0.5%.
Discussion: Literature review revealed 22 total cases. The mean age was found to be 37.5 years, and mean survival after development of a brain metastasis was 9.9 months.
Conclusion: Brain metastases from MPNSTs are very rare and represent a poor prognosis, with survival after brain metastasis reported to be approximately 10 months. Early and effective initial diagnosis and treatment of MPNSTs likely represent the best opportunity for increased overall survival.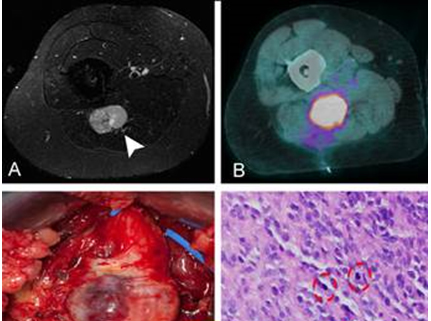
Figure 1. (A) T1-weighted, fat-saturation MRI scan with gadolinium demonstrating a heterogeneous mass arising from the sciatic nerve (arrowhead). (B) Avid FDG-PET uptake. (C) Intraoperative photograph demonstrating uniform enlargement of the sciatic nerve. (D) Pathologic specimen demonstrating a highly cellular tumor with multiple mitotic figures (circles).
Figure 2. En-bloc resection.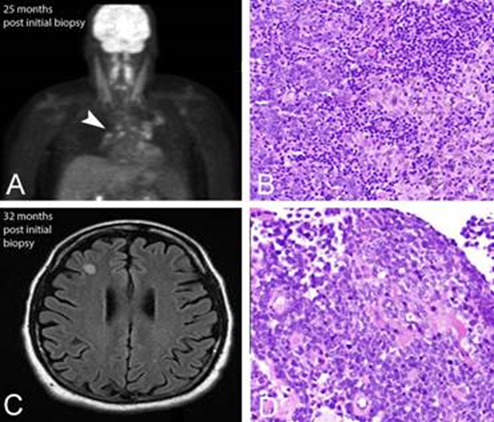
Figure 3. (A) Follow-up PET scan demonstrated evidence of FDG uptake within the peri-hilar lymph nodes. (B) Peri-hilar lymph node biopsy demonstrating evidence of metastatic MPNST. (C) An MRI was performed for new onset left sided symptoms demonstrating a non-enhancing mass in the right frontal lobe on T2-weighted FLAIR sequence. (D) Subsequent brain biopsy pathologic specimen again demonstrates metastatic MPNST.
Back to 2017 Annual Meeting Program
