Back to 2017 Annual Meeting Program
Variables Associated with Outcomes in Peripheral Nerve Repair
Beina Azadgoli, MS; Don Hoang, MD, MHS; Hyuma A Leland, MD; Nana-Yaw Bonsu, BS; Joseph Carey, MD
Keck School of Medicine, University of Southern California, Los Angeles, CA
Background: Data regarding outcomes after peripheral nerve injuries is limited, and the optimal management strategy for an acute injury is unclear. The aim of this study was to examine specific patient and surgical factors that impact motor and sensory outcomes after peripheral nerve injury.
Methods: This was a single center, retrospective study at a metropolitan level 1 trauma center. Patients with traumatic peripheral nerve injury from 01/2010 – 06/2015 were included. Patients who died, required amputation, suffered brachial plexus injury, or had missing motor-sensory exams were excluded. Motor and sensory exams were graded 0-5 by the Modified British Medical Research Council system. Operative repair of peripheral nerves was analyzed for patient characteristics, anatomic nerve injury, level of injury, associated injuries, days until repair, and repair method.
Results: 311 patients met inclusion criteria. 258 (83%) patients underwent operative management, and 53 (17%) underwent non-operative management. Those who required operative intervention had significantly more penetrating injuries 85.7% vs 64.2% (p<0.001), worse initial motor scores 1.19 vs 2.23 (p=0.004), and worse initial sensory exam scores 1.75 vs 2.28 (p=0.029). Predictors of improved operative motor outcomes on univariate analysis were Injury Severity Score (ISS) <15 (p=0.013), male sex (p=0.006), while upper arm level of injury was a predictor (p=0.041) of poor outcome. Nerve reconstruction type between primary, allograft, autograft, or nerve tube did not influence motor outcomes (p=0.15). Multivariate analysis did not confirm level of nerve injury to be predictive of outcome. Univariate analysis identified distal forearm level of injury (p=0.026) and autograft repair (p=0.048) as predictors of poor sensory outcome. These variables were not found to be significant on multivariate analysis. Days to nerve repair (² 24 hours versus >24 hours, p=0.834) did not influence motor-sensory outcome.
Conclusion: Outcomes were primarily influenced by patient characteristics, and injury level to a lesser degree, rather than operative repair characteristics. 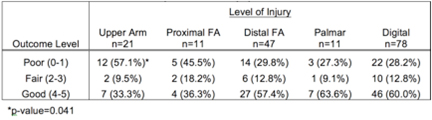
Table 1. Outcomes: Motor Recovery and Level Injury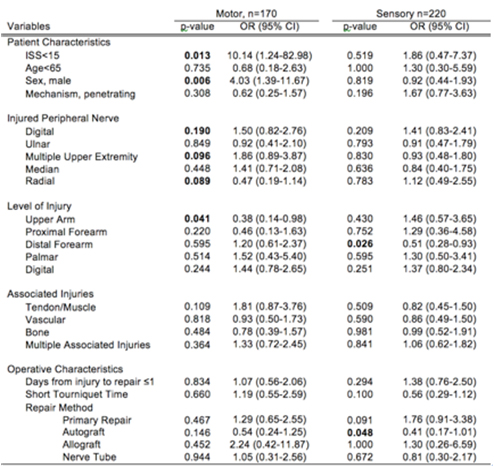
Table 2. Predictors of Improved Motor-Sensory Outcomes: Univariate Analysis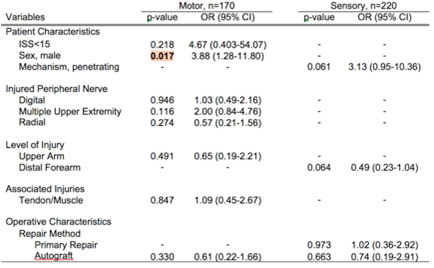
Table 3. Predictors of Improved Motor and Sensory Outcomes: Multivariate Analysis
Back to 2017 Annual Meeting Program
