Optimizing Exposure for the Occipital Nerve in Migraine Surgery while Maintaining Hair Length
Kevin Jubbal, BS; Anthony Echo, MD
Houston Methodist Hospital, Houston, TX
Introduction: Occipital trigger sites for migraine headaches exist in a significant proportion of patients with migraine, almost all of whom experience an improvement in symptoms after surgical decompression of the greater occipital nerve (GON)1,2. In order to gain access to the GON, third occipital nerve (TON), and/or lesser occipital nerve (LON), a midline incision is made at the occiput. The patient's hair is shaven or trimmed preoperatively approximately 2cm in width3. While this may reduce obstruction, it results in an unappealing variation in hair length resembling a reverse mohawk that may take several weeks or months to resolve. Guidelines state it is best to avoid preoperative hair removal when possible to reduce the rates of surgical site infection4,5. We suggest an alternative approach whereby the hair is parted and secured away from the surgical site using sterile surgical tape (Fig. 1, 2) resulting in a more natural outcome (Fig. 3). The purpose of this study is to promote the use of this alternative method when accessing the GON during surgical decompression in order to both improve patient satisfaction and decrease theoretical risk of surgical site infection.
Materials & Methods: We performed a retrospective analysis of all occipital nerve decompression surgeries for the treatment of migraine between the years of 2014 and 2016 at an academic medical center.
Results: A total of 16 patients were identified (Table 1). All 16 patients underwent decompression of the GON, 13 patients (81%) underwent transection of the TON, 11 patients (69%) underwent neurolysis of the LON, and 2 patients (13%) underwent lipoma excision through the occipital approach. Additionally, 5 patients (31%) underwent surgical treatment at the supraorbital nerve (SON), 4 patients (25%) underwent treatment at the supratrochlear nerve (STN), 5 patients (31%) underwent treatment at the zygomaticotemporal branch of the trigeminal nerve (ZGTBTN), and 1 patient (6%) underwent treatment at the auriculotemporal nerve (AT). One patient (6%) developed surgical site superficial cellulitis which was resolved with a standard course of antibiotic therapy.
Conclusions: The securing of occipital hair with surgical tape instead of preoperative hair removal is a viable alternative in the surgical approach for GON decompression. The preservation of hair length will increase patient satisfaction, and avoidance of preoperative hair removal reduces the theoretical risk of surgical site infection.

Figure 1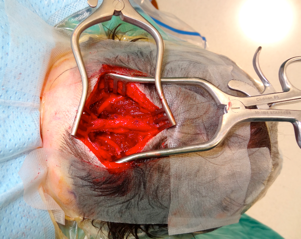
Figure 2
Figure 3
Back to 2017 ePoster Listing
