Back to 2017 Annual Meeting Program
Primary Targeted Reinnervation for the Amputee - Can Painful Neuroma and Phantom Limb Pain be Prevented?
John Byers Bowen, MD, MS; Corinne Wee, BS; Ian L. Valerio, MD, MS, MBA
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction
About 25% of major limb amputees develop chronic localized painful neuroma (PN) and phantom limb pain (PLP). Previous studies prove TR successfully treats and, in some cases, resolves PN and PLP in patients whom have undergone previous amputation (i.e. secondary TR). This study examines the incidence of PN, PLP, and associated outcomes when TR is performed at the time of initial amputation (i.e. primary TR).
Methods
A retrospective review of all patients that underwent primary TR at our institution was completed. Each patient had his or her major amputated mixed motor-sensory and sensory peripheral nerves identified at his index amputation surgery. A nerve stimulator was utilized to identify proximal motor nerves entering specific muscle units. These target motor nerves were divided near their associated uscle and the prior amputated nerves were coapted to the target motor nerve. Subjects were followed at one, three, six, and twelve-month intervals to evaluate symptoms of PN, PLP, phantom limb sensation, patient satisfaction, and functionality.
Results
Fourteen patients have been treated with primary TR. Operative details and follow-up reports of PN and PLP are shown (Table 1). Thus far, one patient reported PN at one month, which resolved by three months. At one month, 64% of patients reported PLP which, in all patients, resolved by three months. By three months, a majority of patients demonstrated targeted specific muscle reanimation with intuitive control of this muscle fasciculation.
Discussion
Improvement of PN and PLP was first noted in upper limb amputee patients undergoing secondary TR in order to improve bio-prostheses intuitive control. Our pilot study suggests that TR can decrease the incidence of PN and PLP when performed at the time of amputation. Our patients demonstrate early muscle fasciculation that suggests better muscle motor end plate function and less disuse/atrophy due to earlier nerve to muscle interface. We have noted trends towards quicker disuse of narcotics potentially due to decreased central nervous feedback. This study expands the use of TR, provides a basis for future studies regarding the specific use of TR to prevent PN and PLP, and also provides patients with the future option for bio-prosthetics.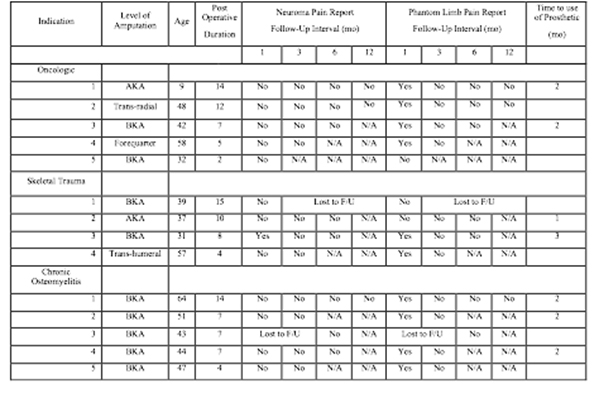
Back to 2017 Annual Meeting Program
