Back to 2017 Annual Meeting Program
Comparison Between Two Collagen Nerve Conduits and Nerve Autograft for Motor Nerve Regeneration in a Rat Model
Eliana Saltzman, BA; Jordan Carolina Villa, MD; Joseph H Feinberg, MD; Steve K Lee, MD; Scott W Wolfe, MD
Hospital for Special Surgery, New York, NY
Introduction: Current synthetic conduits fail to provide equivalent motor recovery compared to autologous nerve repairs of peripheral nerve injuries. Autograft repairs are additionally associated with donor site morbidity and are limited by tissue availability. A synthetic conduit that enables equivalent motor recovery would thus provide an ideal graft alternative. A novel polyglycolic acid conduit (Nerbridge, Toyobo Co., Ltd., Osaka, Japan), uniquely contains collagen fibers within the tube to provide support and guidance for regenerating peripheral nerves through the transected site. We hypothesized that this collagen-filled conduit would generate motor recovery equivalent to that of autograft, and superior to a hollow collagen conduit (NeuraGen nerve guide, Integra, Plainsboro, NJ) as a result of its internal scaffold.
Methods: 72 Lewis rats were randomized into 3 experimental groups, in which a unilateral 10-mm sciatic defect was repaired using nerve autograft, collagen-filled conduit, or hollow collagen conduit. Outcomes were measured at twelve and sixteen weeks postoperatively, and included bilateral tibialis anterior muscle weight, voltage and force maximal contractility, assessment of ankle contracture, and nerve histology. Results were expressed as a percentage of recovery from the contralateral side. Kruskal-Wallis analysis was utilized with an alpha level of p < 0.05 to determine significance, and post-hoc Bonferroni-correction was used for multiple comparisons.
Results: At twelve weeks, mean muscle force compared to that of the contralateral control side was 50% ±21 for autograft, 9% ±6 for the collagen filled conduit, and 32% ±21 for the hollow collagen conduit. After sixteen weeks, the mean muscle force was 72.4% ±22.5 for autograft, 58.0% ±19.3 for collagen-filled conduit, and 61.1% ±24.8 for collagen hollow conduit. Autograft was statistically superior to both conduits for all outcomes except histology (Fig 1). The conduits demonstrated equivalence to each other across outcomes. Although all three groups experienced improved outcomes from twelve to sixteen weeks, the collagen filled conduit demonstrated the greatest rate of recovery in axonal density over this period.
Conclusion: Autograft repair provided superior motor recovery than the use of two distinct collagen conduits for a 10-mm nerve gap in a rat model. Nevertheless, the collagen filled conduit demonstrated encouraging improvement in muscle force and axon density between 3 and 4 months postoperatively, highlighting its utility in spanning nerve gaps, particularly when autograft is unavailable. 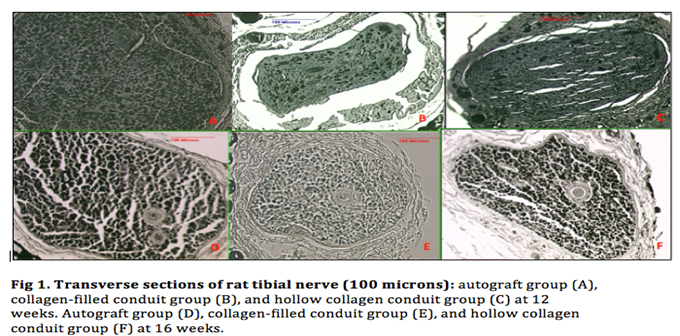
Back to 2017 Annual Meeting Program
