Back to 2017 Annual Meeting Program
Recovery of Elbow Flexion After Delayed Nerve Reconstruction versus Free Functional Muscle Transfer for Traumatic Brachial Plexus Palsy: A Systematic Review
Don Hoang, MD, MHS; Vivi W Chen, BS; Mitchel Seruya, MD
Keck School of Medicine, University of Southern California, Los Angeles, CA
Purpose: In delayed presentation of brachial plexus trauma, the question arises as to whether donor nerves should be devoted to nerve reconstruction or reserved for free functional muscle transfer (FFMT). The purpose of this study was to systematically review recovery of elbow flexion after delayed nerve reconstruction versus FFMT for traumatic brachial plexus palsy.
Methods: A systematic review was performed using the PUBMED, SCOPUS, and Cochrane databases in order to identify all cases of traumatic brachial plexus palsy in patients 18 years or older. Patients who underwent delayed (>=12 months) nerve reconstruction or FFMT for elbow flexion were included. Demographics were recorded, including age, time to operation, and level of brachial plexus injury. Functional outcomes were evaluated, including British MRC strength and range of motion for elbow flexion.
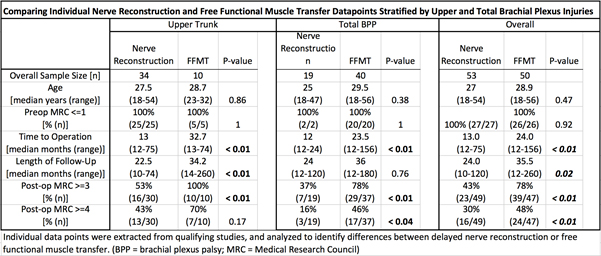
Results: Thirty-three studies met criteria (Figure 1) for a total of 103 patients (53 delayed nerve reconstruction, 50 FFMT). The methodological quality of included studies (MINORS) ranged from 50-92%, with a median MINORS criteria score of 54% (IQR 54-71%) for nerve reconstruction and 54% (IQR 54-56%) for FFMT articles (p=0.72). Surgical age and preoperative elbow flexion were no different across the groups, whereas time to surgery and follow-up time were significantly longer in the FFMT group (Table 1). For upper trunk injuries, 53% of nerve reconstruction patients versus 100% of FFMT patients achieved M3 or greater strength (p<0.01) and 43% of nerve reconstruction patients versus 70% of FFMT patients achieved M4 or greater strength (p=0.17). In total brachial plexus injuries, 37% of nerve reconstruction patients versus 78% of FFMT patients achieved M3 or greater strength (p<0.01) and 16% of nerve reconstruction patients versus 46% of FFMT patients achieved M4 or greater strength (p<0.04).
Conclusion: In delayed presentation of traumatic brachial plexus injuries, donor nerves should be reserved for free functional muscle transfer rather than for nerve reconstruction to restore elbow flexion.
Figure 1. Attrition diagram for systematic review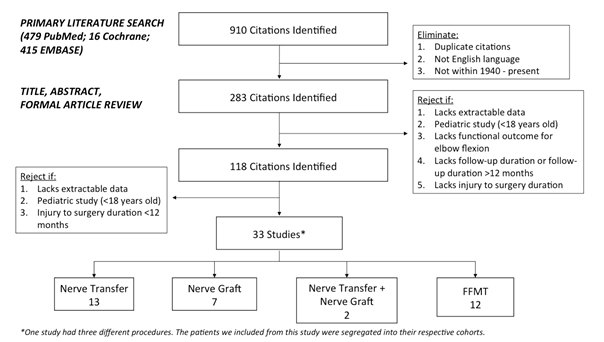
Back to 2017 Annual Meeting Program
