Back to 2017 Annual Meeting Program
Combined Nerve Transfers for Facial Paralysis
Nobutaka Yoshioka, MD
Tominaga Hospital, Osaka, Japan
Background: Although various nerve transfers have been reported as the treatment for the patients with facial paralysis who still have vital facial musculature without available proximal facial nerve stumps, an ideal nerve transfer for reanimating the face has not yet been established. The author has performed combined nerve transfers to the separate distal facial nerve branches with concomitant staged cross-face nerve graft for the patients with reversible facial paralysis with aim of acquiring symmetry at rest, minimizing synkinesis, , and spontaneous smile.
Patients and methods: From May 2013 to October 2015, seven patients with unilateral facial paralysis were treated with this technique. The ages of the patients ranged from 14 to 71 years (mean: 48 years). Five patients had modified House-Brackmann grade 6 facial nerve function and two had grade 5 preoperatively. The etiology of facial paralysis was extirpation of the brain tumor in six patients and Hunt syndrome in one. Duration of paralysis was between 4 months and 27 months (median: 9). All patients underwent masseteric nerve transfer to the main zygomatic branch of the facial nerve and direct or indirect mini-hypoglossal nerve transfer to the lower trunk of the facial nerve. Concomitant staged cross-face nerve graft between the both zygomatic branches was intended to reconstruct smiling (Figure 1). Secondary neurorrhaphy between the cross-face nerve graft and distal branches of the main zygomatic branch in the affected side was performed with the previously performed masseteric to the main zygomatic branch coaptation being left intact.
Results: The follow-up period after the secondary neurorrhaphy was between 3 and 24 months (mean: 12months). Five patients had modified House-Brackmann grade 4 function and two patients had grade 3 function. Every patient achieved nearly symmetrical resting symmetry and voluntary elevation of the corner of the mouth with minimal synkinesis. No spontaneous smile was acquired in every patient during the follow-up period.
Conclusions: Among various nerve transfer techniques, combined masseteric and mini-hypoglossal nerve transfers to the separate distal facial nerve branches provide reliable dynamic facial reanimation, resting symmetry, and minimal synkinesis. Further follow-up is necessary to evaluate the synchronized movement of the corners of the mouth and spontaneous smiling. 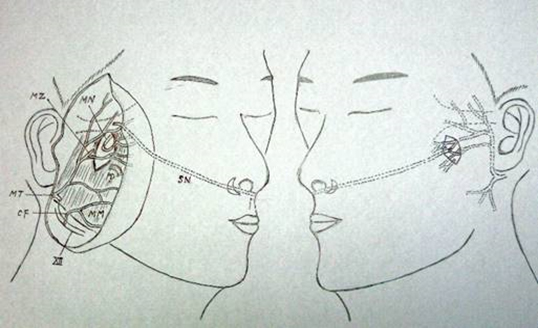
(Figure 1 ) MN: masseteric nerve, MZ: main zygomatic branch, PD: parotid duct, MT: main trunk, CF: cervicofacial trunk, MM: masseter muscle, SN: sural nerve
Back to 2017 Annual Meeting Program
