Back to 2017 Annual Meeting Program
Investigation into the Optimal Number of Intercostal Nerve Transfers for Musculocutaneous Nerve Re-Innervation
Hyuma A. Leland, MD; Daniel J. Gould, MD, PhD; Mitchel Seruya, MD
Keck School of Medicine of the University of Southern California, Los Angeles, CA
Introduction: Intercostal nerve transfer is one approach to neurotize the musculocutaneous nerve in brachial plexus injury. This study investigates outcomes following intercostal nerve transfer with a primary focus on the number of nerve transfers required to achieve optimal return of elbow flexion.
Methods: A systematic review of the literature was performed in accordance with PRISMA guidelines searching the MEDLINE/Pubmed and Google Scholar databases. Studies investigating intercostal nerve transfer for musculocutaneous innervation following brachial plexus injury in adults were included. Citations were cross-referenced and relevant studies included for analysis. All studies evaluated return of motor function based on the British Medical Research Council scale for muscle strength. Statistics were calculated using weighted means and the student's t test with α ≤ 0.05. With β = 20%, power calculations demonstrated a minimum of 25 patients per study arm.
Results: Nine studies were included for analysis. A total of 641 patients were analyzed with average age 24.9 ± 5.4 years and 93% male population. The average time to surgery was 4.0 ± 1.5 months with average follow up of 41.3 ± 3.7 months. One study reported a single intercostal transfer resulting in restoration of M3 strength elbow flexion. Eight studies reported transfer of 2 intercostals in 414 patients with 76.6% of patients achieving ≥ M3 flexion. Six studies reported transfer of 3 intercostals in 218 patients with 62.4% of patients achieving ≥ M3 flexion. Finally, 6 (87.5%) of the 8 patients who underwent 4 intercostal nerve transfers achieved ≥ M3 flexion. There was no statistically significant difference in return of ≥M3 function between 2 vs. 3 transfers (p = 0.4), 2 vs. 4 transfers (p = 0.4), and 3 vs. 4 transfers (p = 0.07). When comparing return of M4 vs. M3 function, more patients developed M4 function when transferring 2 intercostal nerves (p = 0.05), but there was no difference when transferring 3 intercostals (p = 0.2).
Conclusion: Intercostal nerve transfer to the musculocutaneous nerve is an operation largely performed in 25-year-old males around 4 months after brachial plexus injury. No significant difference in return of ≥M3 elbow flexion was demonstrated with increased transfer of intercostal nerves. Based on equivalent outcomes, transfer of 2 intercostal nerves is recommended.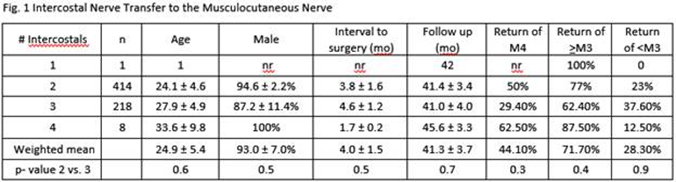
Back to 2017 Annual Meeting Program
