Back to 2015 Annual Meeting Program
Evaluation of Viability and Structural Integrity after Whole Eye Transplantation
Yang Li, MD, PhD1; Chiaki Komatsu, MD1; Bo Wang, BS1; Nataliya Kostereva, PhD1; Wensheng Zhang, MD, PhD1; Bo Xiao, MD, PhD1; Mario Solari, MD1; Jeffrey Goldberg, MD, PhD2; Larry Benowitz, PhD3; Larry Kagemann, PhD1; Shuzhong Guo, MD, PhD4; Gadi Wollstein, MD1; Joel Schuman, MD1; Vijay S. Gorantla, MD, PhD1; Kia Washington, MD1
1University of Pittsburgh; 2University of California San Diego; 3Harvard University; 4Fourth Military Medical University
BACKGROUND: Approximately 37 million people throughout the world suffer from blindness. Whole eye transplantation (WET) gives the opportunity to provide viable retinal ganglion cells and the entire optical system to recipients with vision loss and irreversible injury to the eye. A key obstacle to WET is the poor regenerative ability of the optic nerve. Recently, several groups have demonstrated optic nerve regeneration, showing promise for eye transplantation. There has been difficulty in establishing a consistent small animal model for basic science research in WET. We previously established and published a functional face transplant model in the rat, and have recently expanded our model to include the whole eye, optic nerve and its blood supply.
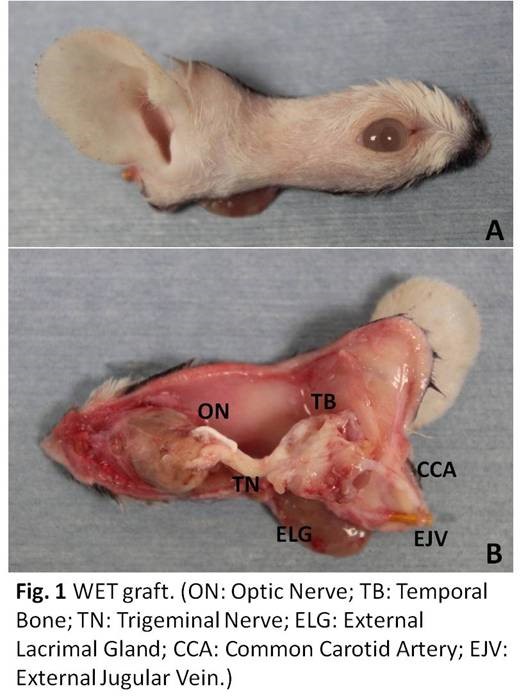
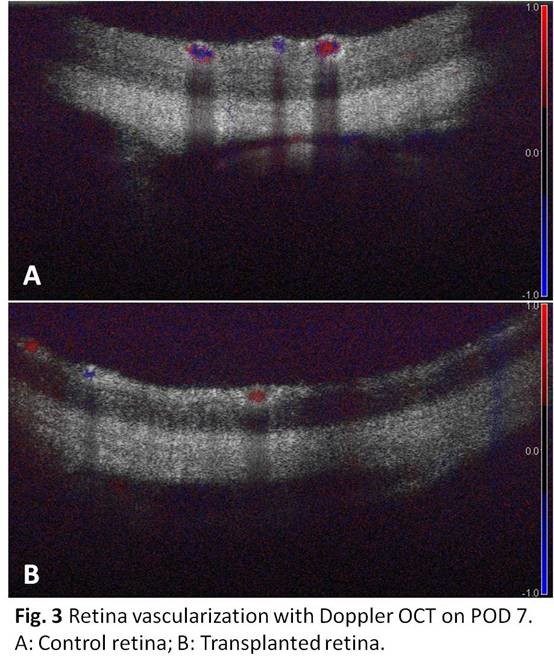
Methods: All syngeneic transplants were performed in Lewis (RT1l) rats. The donor flap, pedicled by the common carotid artery and external jugular vein, is composed of all ocular tissue distal to the optic chiasm, a portion of the temporal bone, and the skin tissues of the eyelids and external ear. The recipient site was prepared by removing a similar region of skin tissue and the eye socket content, with the optic nerve cut at the base of the globe. A nerve apposition between the donor and recipient optic nerve was performed. Slit lamp examination and Optical coherence tomography (OCT) imaging of the cornea, lens and retina were performed weekly after transplantation. Histological sections of the eye were analyzed post-mortem.
Results: 6 out of 8 rats survived the surgical procedure while maintaining visual transparency of the anterior eye. All eyes were viable via slit lamp examination. OCT imaging confirmed transparency of the cornea and lens, preservation of the structural layers of the retina, and blood flow throughout the eye. Histology confirmed neovascularization of the cornea as well as preservation of the structural integrity of the retina, with the exception of degeneration of the retinal ganglion cell layer.
Conclusion: We have established a viable orthotopic model for vascularized whole eye transplantation in the rat. Maintenance of structural integrity and viability were confirmed by slit lamp examination, OCT, and histology. The model is ideal for examining viability, functional return and immunology in whole eye transplantation.
Figures

Back to 2015 Annual Meeting Program
