Back to 2015 Annual Meeting Program
Corneal Reinnervation: A Minimally Invasive Approach
Joseph Catapano, MD; Uri Elbaz, Robert Bains, MD; Ronald M. Zuker, MD; Asim Ali, MD; Gregory H. Borschel, MD
Division of Plastic and Reconstructive Surgery, University of Toronto, Toronto, ON, Canada
Introduction: Corneal sensation is a necessary component of corneal maintenance. Corneal anesthesia renders the cornea susceptible to non-healing epithelial ulceration, scarring and perforation. Previously, unilateral corneal reinnervation has been achieved with direct neurotization using the contralateral supraorbital and supratrochlear nerves. However, this technique requires an extensive dissection and bicoronal incision. We present the early results of a less invasive corneal neurotization technique in young patients.
Materials & Methods: An end-to-side coaptation was performed from the donor supratrochlear nerve to a sural nerve graft. The graft was tunneled subconjunctivally to the perilimbal area and draped around the cornea. Corneal anesthesia was evaluated preoperatively and postoperatively in the center of the cornea and in four corneal quadrants using a Cochet-Bonnet esthesiometer.
Results: Preoperatively, all corneas sustained complications related to corneal anesthesia and lacked any detectable sensation preoperatively. Five eyes underwent the procedure (aged 9-34 years), with one patient undergoing bilateral reconstruction. Figure 1 shows the time progression of the esthesiometry measurements in the four pediatric eyes completed to date, with A and B representing the patient with bilateral reconstruction. A score of 60 is considered indistinguishable from normal, and a score of 15 is required for protective corneal sensation. No complications occurred postoperatively. The adult patient, aged 34, is demonstrating improved corneal sensation 6 months post-operatively.
Conclusions: Corneal sensory reconstruction restores corneal sensation and ocular defense mechanisms, protecting vision in patients with previously anesthetic corneas. This can be achieved with minimal morbidity using sural nerve grafts and this novel method avoids the cosmetically objectionable bicoronal scar. This is the first report of restoration of corneal sensation using a sural nerve graft for unilateral and bilateral anesthetic corneas. Furthermore, this technique may enable future corneal transplantation in patients with irreversible corneal scarring.
Figure 1: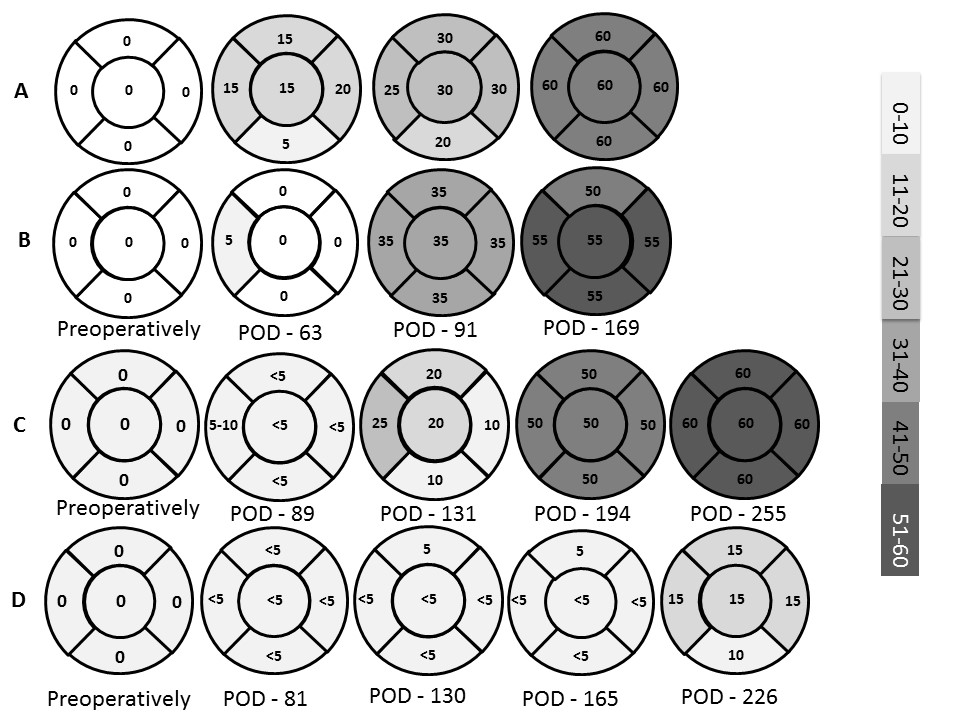
Back to 2015 Annual Meeting Program
