Back to 2015 Annual Meeting Program
The Psychological Impact of Brachial Plexus Injury
Zoe Ambre Landers, LCSW1; Steve K. Lee, MD2 ; Carol A. Mancuso, MD, FACP3; Scott W. Wolfe, MD2
1Center for Brachial Plexus and Traumatic Nerve Injury & Department of Social Work Programs, Hospital for Special Surgery, New York, NY; 2Hand and Upper Extremity Surgery, Hospital for Special Surgery, New York, NY; 3Department of Medicines, Hospital for Special Surgery, New York, NY
Introduction: We hypothesized that brachial plexus injury (BPI) profoundly impacts patients psychologically. To inform, improve upon and develop standard best practices for multidisciplinary treatment of BPI this pilot study collected clinical data about the psychological effects of BPI, specific patient psychosocial concerns and associated sources of psychological distress, and subsequent impact on daily functioning.
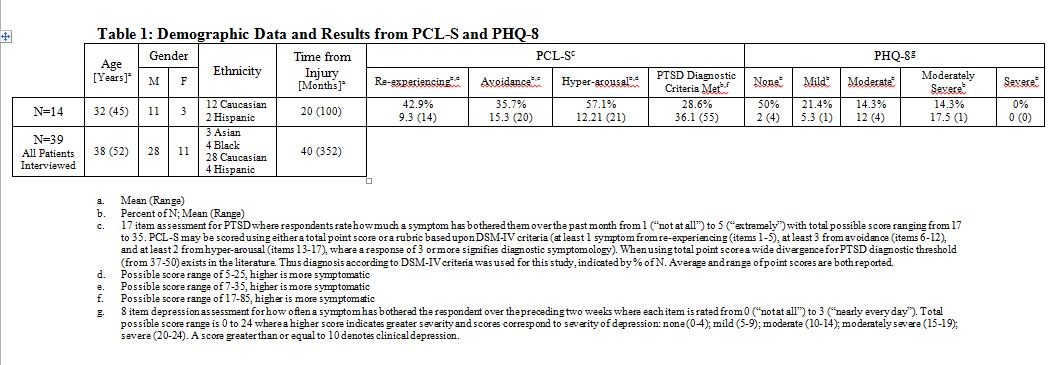
Materials & Methods: Between February 2013 and January 2014 during scheduled pre-operative surgical assessments and/or post-operative appointments, the staff social worker at a major brachial plexus center conducted mixed-methods psychosocial interviews with 39 patients to assess impact of BPI on psychological functioning. Open-ended interview questions explored how BPI affected perception of self and ability to function in interpersonal, familial, occupational, discretionary, and necessary daily living situations. Further questions investigated how adapting to and accepting BPI influenced mood and variance thereof over time. Patients (n=14) were evaluated for posttraumatic stress disorder (PTSD), depression, and substance use through the respective validated scales: Post Traumatic Stress Disorder Checklist-Specific (PCL-S) Patient Health Questionnaire-8 (PHQ-8), National Institute on Drug Abuse Quick Screen (NIDA Quick Screen).
Results: Mean age was 38 and 71.8% were men. BPI strongly impacted psychological well-being as evidenced by patient report and higher prevalence of PTSD and depression than US population norms (6.8% and 16.6% respectively). Open-ended interview questions revealed sources of psychological distress ranging from substantial negative impact on self-worth, to increased dependency upon others, to loss of employment. Results of the PCL-S and PHQ-8 supported clinical data from interviews (Table 1). 28.6% met diagnostic criterion for PTSD. Although 50% showed symptoms of depression, only 28.6% exhibited clinical depression. Of the 39 interviewed, 20.5% divulged suicidal thoughts. Consistent with other studies investigating the impact of comorbid PTSD and depression on suicidality, severity of suicidal ideation was most prevalent in depressed patients currently experiencing PTSD. Patients disclosed social alcohol and tobacco use but no significant substance abuse patterns were noted.
Conclusions: BPI significantly influences psychological well-being and ability to function in daily life. In addition there is a high prevalence of PTSD, depression, and suicidal ideation as a result of BPI. Subsequently, BPI patients have unique psychosocial concerns and psychological challenges requiring continued psychological attention throughout treatment and further study to develop multidisciplinary standard best practices for comprehensive BPI treatment.
Back to 2015 Annual Meeting Program
