Back to 2015 Annual Meeting Program
Impact of Age on Outcomes in Peripheral Nerve Repair with Processed Nerve Allograft
Bauback Safa, MD1; Renata V. Weber, MD2; Brian Rinker, MD3; John Ingari, MD4; Jason Ko, MD5; Jozef Zoldos, MD6; Gregory A. Merrell, MD7; Jeffrey A. Greenberg, MD, MS8; Wesley Thayer, MD, PhD9; Mickey S. Cho, MD10; Gregory Buncke, MD1
1The Buncke Clinic, San Francisco, CA; 2Institute for Nerve, Hand, and Reconstructive Surgery, Rutherford, NJ; 3Division of Plastic Surgery, University of Kentucky, Lexington, KY; 4WellSpan Health Orthopedics, York, PA; 5Division of Plastic and Reconstructive Surgery, University of Washington, Harborview Medical Center, Seattle, WA; 6Arizona Center for Hand Surgery, Phoenix, AZ; 7Department of Orthopaedic Surgery & Rehabilitation, Indiana Hand to Shoulder Center, Indianapolis, IN; 8The Indiana Hand to Shoulder Center, Indianapolis, IN; 9Department of Plastic Surgery, Vanderbilt University, Nashville, TN; 10Department of Orthopedics & Rehabilitation, San Antonio Military Medical Center, San Antonio, TX
Introduction: Many factors that are outside of the surgeon's control impact the level of functional recovery following peripheral nerve repair. These factors include age of the patient, mechanism of injury, location of injury, and demographical background. Recent meta-analyses have reported that average functional recovery rates for adults can decrease by 50% in patient over 50, as compared to those under 30. The cause of these decreases are not well characterized, however age related changes in regenerative potential and decreased cortical plasticity are thought to play a role. To determine the impact of patient age on the outcomes from the use of processed nerve allograft, the RANGER registry database was queried and results stratified by subject age.
Materials & Methods: IRB approval was obtained and standardized data reports were used to collect utilization, safety and functional outcomes. Follow-up evaluations included 2-point discrimination, Monofilament testing, range of motion, electromyography, force testing, MRCC scores and safety assessments. Covariate analysis were performed to further characterize the sub-groups. Meaningful recovery was defined by the MRCC scale at S3/M3 or greater for sensory and motor function in all groups. Complex mechanisms of injury included avulsions, amputations, blasts and high energy injuries.
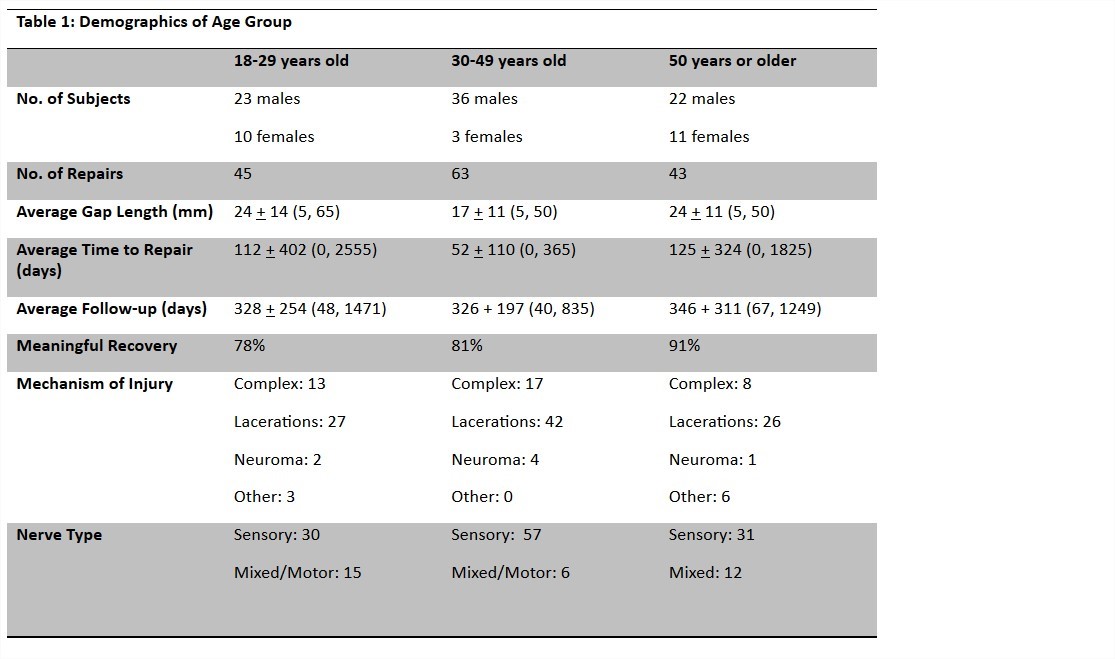
Results: Sufficient outcomes data was reported for 109 subjects with 151 nerve repairs. The subjects were placed into three age groups: 18-29, 30-49, and 50 years of age or older. Overall meaningful recovery rates were 78%, 81% and 91% respectively. Table 1 provides the breakdown of the demographics of each group. The groups were evenly distributed by gap length, injured nerve and time to repair. The 18-29 group contained 62% more complex injuries than the 50+ group. The 18-29 group contained a majority of the manual labor/construction workers and twice as many military injuries. There were no reported nerve related adverse events.
Conclusion: In this population, patient age did not have a significant impact on functional outcomes. The 50+ year old population did show trends toward a lower incidence of complex traumas and high energy injuries, as compared to the 18-29 group. Processed nerve allografts performed well regardless of age, and can be considered as part of the treatment algorithm independent of patient age. The RANGER® registry is in open enrollment and will continue to collect clinical data to analyze outcomes from nerve repairs.
Back to 2015 Annual Meeting Program
